Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Rate of caesarean sections is higher in endometriosis patients – experience of single tertiary obstetric clinic in the light of epidemiologic data
1
Clinic of Surgical and Oncologic Gynecology, 1st Department of Gynaecology and Obstetrics, Medical University of Łódż, M. Pirogow’s Teaching Hospital, Poland
2
Clinic of Foetal Medicine and Gynecology, 1st Department of Gynaecology and Obstetrics, Medical University of Łódż, M. Pirogow’s Teaching Hospital, Poland
3
Student Scientific Society, 1st Department of Gynaecology and Obstetrics, Medical University, Łódż, Poland
Corresponding author
Susan Afshari-Stasiak
Clinic of Surgical and Oncologic Gynecology, 1st Department of Gynecology and Obstetrics, Medical University of Lodz, M. Pirogow’s Teaching Hospital, Wilenska 37, 94-029, Lodz, Poland
Clinic of Surgical and Oncologic Gynecology, 1st Department of Gynecology and Obstetrics, Medical University of Lodz, M. Pirogow’s Teaching Hospital, Wilenska 37, 94-029, Lodz, Poland
J Pre Clin Clin Res. 2023;17(2):56-61
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Endometriosis is defined as the presence of endometrium-like tissue outside the uterine cavity which can cause chronic pelvic pain, dysmenorrhea, infertility, and obstetric complications. The study was undertaken to elucidate the influence of endometriosis on conception, pregnancy and course of Latour, as well as outcomes for the growth of the foetus.
Material and methods:
A single centre study was undertaken of endometriosis patients who were followed-up for five years after laparoscopy. The study group consisted of 30 patients with endometriosis who conceived, of whom 120 underwent laparoskopy. The control group consisted of 30 healthy women who delivered children and were hospitalized in a two-month period in 2015. Each patient completed a questionnaire regarding endometriosis symptoms, infertility duration, gravidity, smoking habits, education, metod of conception, incidence of pre-term labour, foetal growth restriction (FGR), small for gestational age (SGA) and pregnancy-induced hypertension (PIH). Analysis of the data was carried out using STATISTICA v.10.
Results:
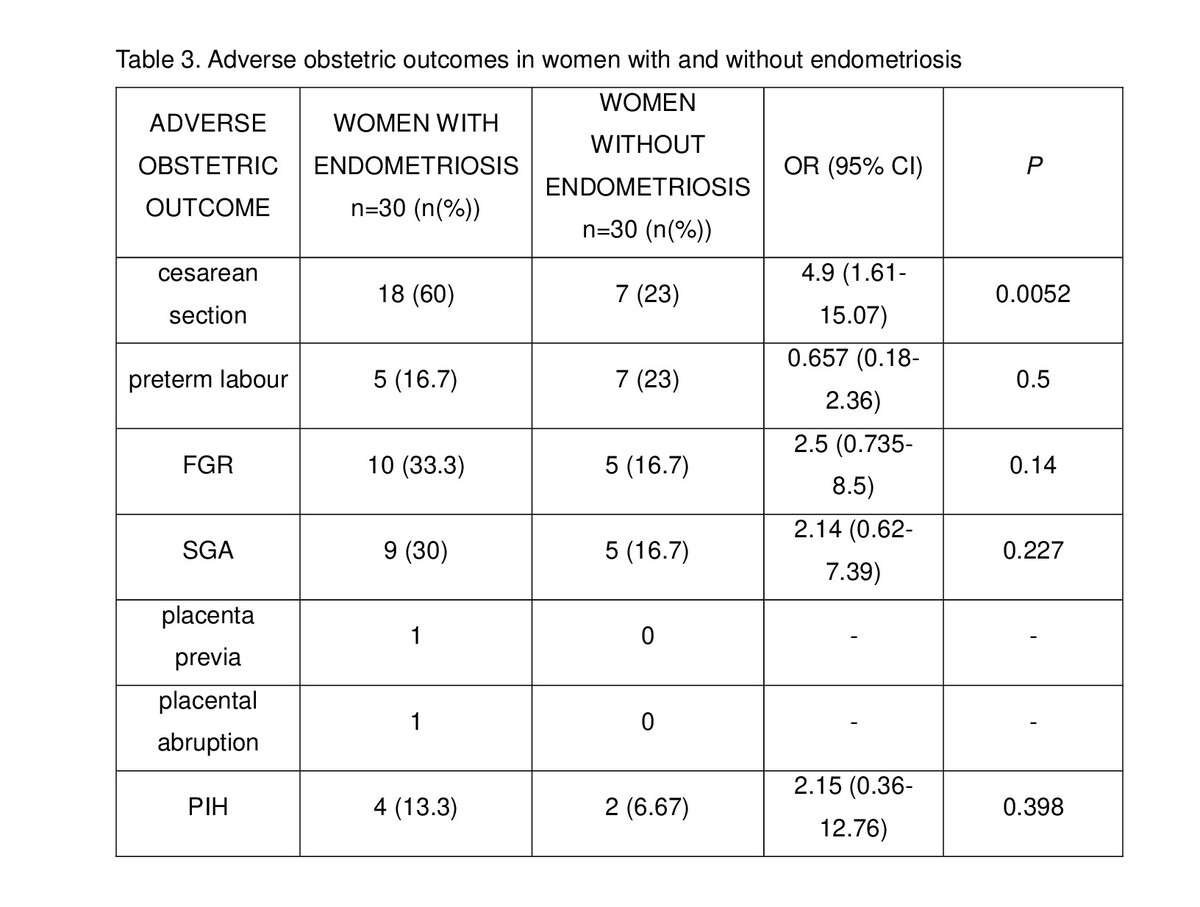
A significant difference was observed in maternal age (34.7 ±4.7 for the study group vs. 29.8±4.9 years for the control group; p=0.001). In the study group, an increased incidence of caesarean section was noted (OR 4.9; 95% CI 1.61–15.07). No significant differences were observed in the incidence of preterm labour, FGR, SGA and PIH.
Conclusions:
Delivering child at older age was observed in the endometriosis group, compared with controls, which suggests that endometriosis extends the time to conceiving. Higher maternal age at delivery and prolonged time to pregnancy may be the factors that influence the rate of caesarean section in endometriosis patients.
Endometriosis is defined as the presence of endometrium-like tissue outside the uterine cavity which can cause chronic pelvic pain, dysmenorrhea, infertility, and obstetric complications. The study was undertaken to elucidate the influence of endometriosis on conception, pregnancy and course of Latour, as well as outcomes for the growth of the foetus.
Material and methods:
A single centre study was undertaken of endometriosis patients who were followed-up for five years after laparoscopy. The study group consisted of 30 patients with endometriosis who conceived, of whom 120 underwent laparoskopy. The control group consisted of 30 healthy women who delivered children and were hospitalized in a two-month period in 2015. Each patient completed a questionnaire regarding endometriosis symptoms, infertility duration, gravidity, smoking habits, education, metod of conception, incidence of pre-term labour, foetal growth restriction (FGR), small for gestational age (SGA) and pregnancy-induced hypertension (PIH). Analysis of the data was carried out using STATISTICA v.10.
Results:
A significant difference was observed in maternal age (34.7 ±4.7 for the study group vs. 29.8±4.9 years for the control group; p=0.001). In the study group, an increased incidence of caesarean section was noted (OR 4.9; 95% CI 1.61–15.07). No significant differences were observed in the incidence of preterm labour, FGR, SGA and PIH.
Conclusions:
Delivering child at older age was observed in the endometriosis group, compared with controls, which suggests that endometriosis extends the time to conceiving. Higher maternal age at delivery and prolonged time to pregnancy may be the factors that influence the rate of caesarean section in endometriosis patients.
ACKNOWLEDGEMENTS
The authoirs extend their special thanks to dr Tomasz Wierzbowski who performed laparoscopies in ednometriosis patients in 2010–2011.
Afshari-Stasiak S, Andrysiewicz S, Andrysiewicz A, Bamberska J, Szubert M. Rate of cesarean sections is higher in endometriosis patients –
experience of single tertiary obstetric clinic in the light of epidemiologic data. J Pre-Clin Clin Res. 2023; 17(2): 56–61. doi: 10.26444/jpccr/163481
REFERENCES (39)
1.
Sorrentino F, Padova DE, Falagario M, et al. Endometriosis and adverse pregnancy outcome. Minerva Obstet Gynecol. 2022;74(1):31–44.10.23736/S2724-606X.20.04718-8.
2.
Eisenberg VH, Weil C, Chodick G, et al. Epidemiology of endometriosis: a large population-based database study from a healthcare provider with 2 million members. BJOG. 2018;125(1):55–62. https://doi.org/10.1111/1471-0....
3.
Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382(13):1244–1256. 10.1056/NEJMra1810764.
4.
Van den Beukel BA, de Ree R, van Leuven S, Bakkum EA, Strik C, van Goor H, et al. Surgical treatment of adhesion-related chronic abdominal and pelvic pain after gynaecological and general surgery: a systematic review and meta-analysis. Hum Reprod Update. 2017;23(3):276–288. https://doi.org/10.1093/humupd....
5.
Ghizzani A, Orlandini C, Bernardi MG, et al. Sexual pain in women: quality of sex life and marital relations. Minerva Ginecol. 2017;69(4):381–389. 10.23736/S0026-4784.17.04054-0.
6.
Lessey BA, Kim JJ. Endometrial receptivity in the eutopic endometrium of women with endometriosis: it is affected, and let me show you why. Fertil Steril. 2017;108(1):19–27. https://doi.org/10.1016/j.fert....
7.
Radwan J, Wołoczyński S. Niepłodność i rozród wspomagany. 1st ed. Poznań: Termedia Wydawnictwo Medyczne; 2011. p. 131–132.
8.
Ibiebele I, Nippita T, Baber R, et al. Pregnancy outcomes in women with endometriosis and/or ART use: a population-based cohort study. Hum Reprod. 2022;37(10):2350–2358. 10.1093/humrep/deac186.
9.
Stern JE, Liu CL, Cui X, et al. Assisted reproductive technology treatment increases obstetric and neonatal risks over that of the underlying infertility diagnosis. Fertil Steril. 2022;117(6):1223–1234. 10.1016/j.fertnstert.2022.02.009.
10.
Lodge-Tulloch NA, Elias FTS, Pudwell J, et al. Caesarean section in pregnancies conceived by assisted reproductive technology: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 21(1):244. 10.1186/s12884-021-03711-x.
11.
Betran AP, Torloni MR, Zhang JJ, et al. WHO Working Group on Caesarean Section. WHO Statement on Caesarean Section Rates. BJOG;123(5):667–70. 1111/1471-0528.13526.
13.
Mechsner S. Endometriose: Eine oft verkannte Schmerzerk rankung [Endometriosis: An often unrecognized pain disorder]. Schmerz. 2016;30(5):477–490. https://doi.org/10.1007/s00482....
14.
Brosens I, Pijnenborg R, Benagiano G. Defective myometrial spiral artery remodelling as a cause of major obstetrical syndromes in endometriosis and adenomyosis. Placenta. 2013;34(2):100–5. https://doi.org/10.1016/j.plac....
15.
Pirtea P, Cicinelli E, De Nola R, et al. Endometrial causes of recurrent pregnancy losses: endometriosis, adenomyosis, and chronic endometritis. Fertil Steril. 2021;115(3):546–560. https://doi.org/10.1016/j.fert....
16.
Fox C, Morin S, Jeong JW, et al. Local and systemic factors and implantation: what is the evidence? Fertil Steril. 2016;105(4):873–884. https://doi.org/10.1016/j.fert....
17.
Chae U, Min JY, Kim SH, Ihm HJ, Oh YS, Park SY, et al. Decreased Progesterone Receptor B/A Ratio in Endometrial Cells by Tumor Necrosis Factor-Alpha and Peritoneal Fluid from Patients with Endometriosis. Yonsei Med J. 2016;57(6):1468–74. https://10.3349/ymj.2016.57.6.....
18.
Riccio LDGC, Santulli P, Marcellin L, et al. Immunology of endometriosis. Best Pract Res Clin Obstet Gynaecol. 2018;50:39–49. 10.1016/j.bpobgyn.2018.01.010.
19.
Kobayashi H, Kawahara N, Ogawa K, et al. A Relationship Between Endometriosis and Obstetric Complications. Reprod Sci. 2020; 27: 771–778. https://doi.org/10.1007/s43032....
20.
Kim SG, Seo HG, Kim YS. Primiparous singleton women with endometriosis have an increased risk of preterm birth: Meta-analyses. Obstet Gynecol Sci. 2017;60(3):283–288. 10.5468/ogs.2017.60.3.283.
21.
Conti N, Cevenini G, Vannuccini S, Orlandini C, Valensise H, Gervasi MT, et al. Women with endometriosis at first pregnancy have an increased risk of adverse obstetric outcome. J Matern Fetal Neonatal Med. 2015;28(15):1795–8. https://doi.org/10.3109/147670....
22.
Li H, Zhu HL, Chang XH, Li Y, Wang Y, Guan J, et al. Effects of Previous Laparoscopic Surgical Diagnosis of Endometriosis on Pregnancy Outcomes. Chin Med J (Engl). 2017;130(4):428–433. 10.4103/0366- 6999.199840.
23.
Zullo F, Spagnolo E, Saccone G, Acunzo M, Xodo S, Ceccaroni M, et al. Endometriosis and obstetrics complications: a systematic review and meta-analysis. Fertil Steril. 2017;108(4):667–672.e5.https://doi. org/10.1016/j.fertnstert.2017.07.019.
24.
Juang CM, Chou P, Yen MS, Twu NF, Horng HC, Hsu WL. Adenomyosis and risk of preterm delivery. BJOG. 2007;114(2):165–9. https://doi. org/10.5468/kjog.2010.53.1.70.
25.
Shin YJ, Kwak DW, Chung JH, Kim MY, Lee SW, Han YJ. The Risk of Preterm Births Among Pregnant Women With Adenomyosis. J Ultrasound Med. 2018;37(8):1937–1943. https://doi.org/10.1002/ jum.14540.
26.
Fernando S, Breheny S, Jaques AM, Halliday JL, Baker G, Healy D. Preterm birth, ovarian endometriomata, and assisted reproduction technologies. Fertil Steril. 2009;91(2):325–30. https://doi.org/10.1016/j. fertnstert.2008.01.096.
27.
Benaglia L, Candotti G, Papaleo E, Pagliardini L, Leonardi M, Reschini M, et al. Pregnancy outcome in women with endometriosis achieving pregnancy with IVF. Hum Reprod. 2016;31(12):2730–2736. https://doi. org/10.1093/humrep/dew210.
28.
Warzecha D, Pietrzak B, Szymusik I, et al. Should the patients with endometriosis be treated as a risk group of pregnancy complications? Single center experience and literature review and literature review. Ginekol Pol. 2020;91(7):383–388. 10.5603/GP.a2020.0084.
29.
Tzur T, Weintraub AY, Arias Gutman O, et al. Pregnancy outcomes in women with endometriosis. Minerva Ginecologica. 2018;70(2):144–149. 10.23736/S0026-4784.17.04123-5.
30.
Lin H, Leng JH, Liu JT, et al. Obstetric outcomes in Chinese women with endometriosis: a retrospective cohort study. Chin Med J (Engl). 2015;128(4):455–8. 4103/0366-6999.151077.
31.
Borisova AV, Konnon SRD, Tosto V, et al. Obstetrical complications and outcome in patients with endometriosis. J Matern Fetal Neonatal Med. 2022;35(14):2663–2677. https://doi.org/10.1080/147670....
32.
González-Comadran M, Schwarze JE, Zegers-Hochschild F, et al. The impact of endometriosis on the outcome of Assisted Reproductive Technology. Reprod Biol Endocrinol. 2017;15(1):8. https://doi. org/10.1186/s12958-016-0217-2.
33.
Yang P, Wang Y, Wu Z, et al. Risk of miscarriage in women with endometriosis undergoing IVF fresh cycles: a retrospective cohort study. Reprod Biol Endocrinol. 2019;17(1):21. https://doi.org/10.1186/ s12958-019-0463-1.
34.
Lalani S, Choudhry AJ, Firth B, Bacal V, Walker M, Wen SW, Singh S, et al. Endometriosis and adverse maternal, fetal and neonatal outcomes, a systematic review and meta-analysis. Hum Reprod. 2018;33(10):1854– 1865. 10.1093/humrep/dey269.
35.
Pérez-López FR, Calvo-Latorre J, Alonso-Ventura V, et al. Health Outcomes, Systematic Analyses (HOUSSAY) Project. Systematic review and meta-analysis regarding the association of endometriosis and preeclampsia in women conceiving spontaneously or through assisted reproductive technology. Pregnancy Hypertens. 2018;14:213–221. 10.1016/j.preghy.2018.01.003.
36.
Wu Y, Chen Y, Shen M, Guo Y, Wen SW, Lanes A, et al. Adverse maternal and neonatal outcomes among singleton pregnancies in women of very advanced maternal age: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):3. doi: https://doi.org/10.1186/s12884....
37.
Kim H, Richards EG. Collateral damage in childbirth: cesarean delivery as a risk factor for endometriosis recurrence. Fertil Steril. 2022;118(6):1088–1089. 10.1016/j.fertnstert.2022.10.022.
38.
Berlac JF, Hartwell D, Skovlund CW, et al. Endometriosis increases the risk of obstetrical and neonatal complications. Acta Obstet Gynecol Scand. 2017;96(6):751–760. 10.1111/aogs.13111.
39.
Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018;15(1):e1002494. https://doi.org/10.1371/journa....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.