Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Awareness of prenatal anxiety disorders among Obstetricians and General Practitioners in Poland – A cross-sectional study
1
Department and Clinic of Psychiatry, Medical University, Wrocław, Poland
Corresponding author
J Pre Clin Clin Res. 2023;17(2):62-69
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Mental health disorders are more prevalent in pregnancy than in the general population. Anxiety disorders in pregnancy, particularly Pregnancy-Related Anxiety (PrA) have multiple negative consequences for the mother and her child. Pregnant patients have multiple visits with their Obstetric-Gynaecologist or General Practitioner, who can start the necessary treatment or refer them to a psychiatrist.
Objective:
The aim our the study is to evaluate the knowledge of General Practitioners and Obstetrician-Gynaecologists about mental health disorders in pregnancy, and to suggest areas of improvement in clinical practice.
Material and methods:
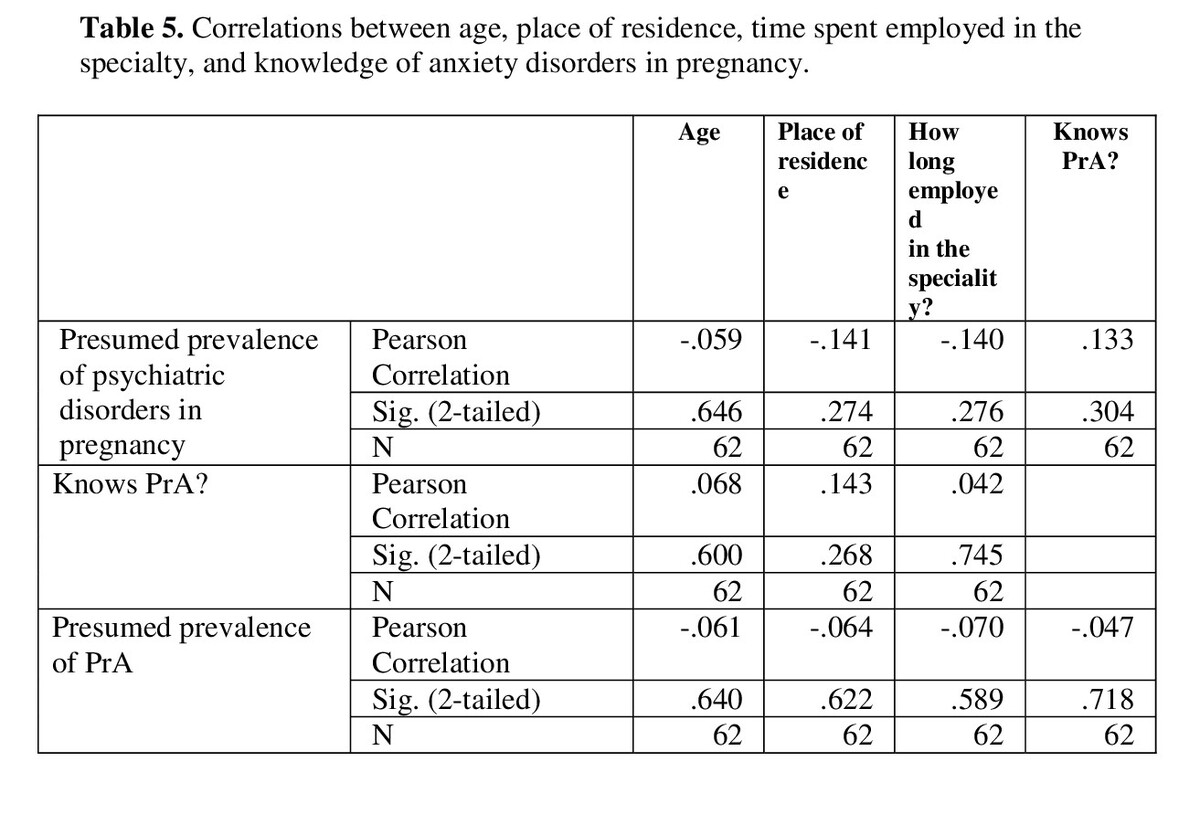
General Practitioners and Obstetricians-Gynaecologists in Poland were asked to complete an online survey consisting of a socio-demographic questionnaire. The questionnaire regarded mental health disorders in pregnancy, and questions regarding anxiety disorders in pregnancy. The results were analysed separately using Pearson correlation calculations for General Practitioners and Obstetrician-Gynaecologists.
Results:
One hundred-one respondents completed an online survey. When asked about the most common disorders in pregnancy, psychiatric conditions were only 5% and 2% of the listed conditions listed by Obstetrician-Gynaecologists and General Practitioners, respectively. 50% of Obstetrician-Gynaecologists and 25% of General Practitioners claimed they were unaware of such conditions as PrA.
Conclusions:
The awareness of mental health disorders, especially Pregnancy-Related Anxiety, among General Practitioners and Obstetricians-Gynaecologists, is inadequate. Improvement in knowledge about antenatal psychiatric conditions is crucial for the well-being of pregnant women and their children.
Mental health disorders are more prevalent in pregnancy than in the general population. Anxiety disorders in pregnancy, particularly Pregnancy-Related Anxiety (PrA) have multiple negative consequences for the mother and her child. Pregnant patients have multiple visits with their Obstetric-Gynaecologist or General Practitioner, who can start the necessary treatment or refer them to a psychiatrist.
Objective:
The aim our the study is to evaluate the knowledge of General Practitioners and Obstetrician-Gynaecologists about mental health disorders in pregnancy, and to suggest areas of improvement in clinical practice.
Material and methods:
General Practitioners and Obstetricians-Gynaecologists in Poland were asked to complete an online survey consisting of a socio-demographic questionnaire. The questionnaire regarded mental health disorders in pregnancy, and questions regarding anxiety disorders in pregnancy. The results were analysed separately using Pearson correlation calculations for General Practitioners and Obstetrician-Gynaecologists.
Results:
One hundred-one respondents completed an online survey. When asked about the most common disorders in pregnancy, psychiatric conditions were only 5% and 2% of the listed conditions listed by Obstetrician-Gynaecologists and General Practitioners, respectively. 50% of Obstetrician-Gynaecologists and 25% of General Practitioners claimed they were unaware of such conditions as PrA.
Conclusions:
The awareness of mental health disorders, especially Pregnancy-Related Anxiety, among General Practitioners and Obstetricians-Gynaecologists, is inadequate. Improvement in knowledge about antenatal psychiatric conditions is crucial for the well-being of pregnant women and their children.
Mikołajkow A, Malaszczak K. Awareness of prenatal anxiety disorders among Obstetricians and General Practitioners in Poland – A cross-
sectional study. J Pre Clin Clin Res. 2023; 17(2): 62–69. doi: 10.26444/jpccr/166112
REFERENCES (57)
1.
Viswasam K, Eslick GD, Starcevic V. Prevalence, onset and course of anxiety disorders during pregnancy: A systematic review and meta analysis. J Affect Disord. 2019;255(5):27–40. doi:10.1016/j.jad.2019.05.016.
2.
Fairbrother N, Janssen P, Antony MM, Tucker E, Young AH. Perinatal anxiety disorder prevalence and incidence. J Affect Disord. 2016;200:148–155. doi:10.1016/j.jad.2015.12.082.
3.
Ahmed A, Feng C, Bowen A, Muhajarine N. Latent trajectory groups of perinatal depressive and anxiety symptoms from pregnancy to early postpartum and their antenatal risk factors. Arch Womens Ment Health. 2018;21(6):689–698. doi:10.1007/s00737-018-0845-y.
4.
Alqahtani AH, Al Khedair K, Al-Jeheiman R, Al-Turki HA, Al Qahtani NH. Anxiety and depression during pregnancy in women attending clinics in a University Hospital in Eastern province of Saudi Arabia: Prevalence and associated factors. Int J Womens Health. 2018;10:101–108. doi:10.2147/IJWH.S153273.
5.
Dikmen-Yildiz P, Ayers S, Phillips L. Depression, anxiety, PTSD and comorbidity in perinatal women in Turkey: A longitudinal population-based study. Midwifery. 2017;55(1):29–37. doi:10.1016/j.midw.2017.09.001.
6.
Fadzil A, Balakrishnan K, Razali R, et al. Risk factors for depression and anxiety among pregnant women in Hospital Tuanku Bainun, Ipoh, Malaysia. Asia-Pacific Psychiatry. 2013;5(1):7-13. doi:10.1111/appy.12036.
7.
Bhushan NL, Krupp K, Jaykrishna P, et al. The association between social support through contacts with Accredited Social Health Activists (ASHAs) and antenatal anxiety among women in Mysore, India: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2020. doi:10.1007/s00127-020-01854-4.
8.
Gourounti K, Anagnostopoulos F, Sandall J. Poor marital support associate with anxiety and worries during pregnancy in Greek pregnant women. Midwifery. 2014;30(6):628–635. doi:10.1016/j.midw.2013.10.008.
9.
Brunton R, Dryer R, Saliba A, Kohlhoff J. Re-examining pregnancy-related anxiety: A replication study. Women and Birth. 2019;32(1):e131–e137. doi:10.1016/j.wombi.2018.04.013.
10.
Theut SK, Pedersen FA, Zaslow MJ, Rabinovich BA. Pregnancy Subsequent to Perinatal Loss: Parental Anxiety and Depression. J Am Acad Child Adolesc Psychiatry. 1988;27(3):289–292. doi:10.1097/00004583-198805000-00004.
11.
Huizink AC, Mulder EJH, Robles De Medina PG, Visser GHA, Buitelaar JK. Is pregnancy anxiety a distinctive syndrome? Early Hum Dev. 2004;79(2):81–91. doi:10.1016/j.earlhumdev.2004.04.014.
12.
Garza-Veloz I, Castruita-De La Rosa C, Ortiz-Castro Y, et al. Maternal distress and the development of hypertensive disorders of pregnancy. J Obstet Gynaecol (Lahore). 2017;37(8):1004–1008. doi:10.1080/01443615.2017.1313823.
13.
Avraham L, Tamar W, Eyal S, Gali P. Perinatal outcomes and offspring long-term neuropsychiatric hospitalizations of mothers with anxiety disorder. Arch Womens Ment Health. 2020. doi:10.1007/s00737-020-01018-y.
14.
Gałazka I, Drosdzol-Cop A, Naworska B, Czajkowska M, Skrzypulec-Plinta V. Does anxiety modify sexuality of pregnant women? Ginekol Pol. 2017;88(12):662–669. doi:10.5603/GP.a2017.0118.
15.
Racine N, Plamondon A, Hentges R, Tough S, Madigan S. Dynamic and bidirectional associations between maternal stress, anxiety, and social support: The critical role of partner and family support. J Affect Disord. 2019;252(12):19–24. doi:10.1016/j.jad.2019.03.083.
16.
Kataja EL, Karlsson L, Huizink AC, et al. Pregnancy-related anxiety and depressive symptoms are associated with visuospatial working memory errors during pregnancy. J Affect Disord. 2017;218:66–74. doi:10.1016/j.jad.2017.04.033.
17.
Grigoriadis S, Graves L, Peer M, et al. A systematic review and meta-analysis of the effects of antenatal anxiety on postpartum outcomes. Arch Womens Ment Health. 2019;22(5):543–556. doi:10.1007/s00737-018-0930-2.
18.
Udry-Jørgensen L, Darwiche J, Germond M, Wunder D, Vial Y. Anxiety, depression, and attachment before and after the first-trimester screening for Down syndrome: Comparing couples who undergo ART with those who conceive spontaneously. Prenat Diagn. 2015;35(13):1287–1293. doi:10.1002/pd.4688.
19.
Nagle-Yang S, Phillips M, Albaugh A, et al. Depression, anxiety, and attachment among women hospitalized on an antepartum unit. Int J Psychiatry Med. 2019;54(6):395–407. doi:10.1177/0091217419837071.
20.
Hopkins J, Miller JL, Butler K, Gibson L, Hedrick L, Boyle DA. The relation between social support, anxiety and distress symptoms and maternal fetal attachment. J Reprod Infant Psychol. 2018;36(4):381–392. doi:10.1080/02646838.2018.1466385.
21.
Hasanjanzadeh P, Faramarzi M. Relationship between maternal general and specific-pregnancy stress, anxiety, and depression symptoms and pregnancy outcome. J Clin Diagnostic Res. 2017;11(4):VC04–VC07. doi:10.7860/JCDR/2017/24352.9616.
22.
Broekman BFP, Chan YH, Chong YS, et al. The influence of anxiety and depressive symptoms during pregnancy on birth size. Paediatr Perinat Epidemiol. 2014;28(2):116–126. doi:10.1111/ppe.12096.
23.
Wallwiener S, Goetz M, Lanfer A, et al. Epidemiology of mental disorders during pregnancy and link to birth outcome: a large-scale retrospective observational database study including 38,000 pregnancies. Arch Gynecol Obstet. 2019;299(3):755–763. doi:10.1007/s00404-019-05075-2.
24.
Blackmore ER, Gustafsson H, Gilchrist M, Wyman C, O’Connor TG. Pregnancy-related anxiety: Evidence of distinct clinical significance from a prospective longitudinal study. J Affect Disord. 2016;197:251–258. doi:10.1016/j.jad.2016.03.008.
25.
Agrati D, Browne D, Jonas W, et al. Maternal anxiety from pregnancy to 2 years postpartum: transactional patterns of maternal early adversity and child temperament. Arch Womens Ment Health. 2015;18(5):693–705. doi:10.1007/s00737-014-0491-y.
26.
Bekkhus M, Lee Y, Nordhagen R, Magnus P, Samuelsen SO, Borge AIH. Re-examining the link between prenatal maternal anxiety and child emotional difficulties, using a sibling design. Int J Epidemiol. 2018;47(1):156–165. doi:10.1093/ije/dyx186.
27.
Bolea-Alamañac B, Davies SJC, Evans J, et al. Does maternal somatic anxiety in pregnancy predispose children to hyperactivity? Eur Child Adolesc Psychiatry. 2019;28(11):1475–1486. doi:10.1007/s00787-019-01289-6.
28.
Adamson B, Letourneau N, Lebel C. Prenatal maternal anxiety and children’s brain structure and function: A systematic review of neuroimaging studies. J Affect Disord. 2018;241:117–126. doi:10.1016/j.jad.2018.08.029.
29.
Dean DC, Planalp EM, Wooten W, et al. Association of Prenatal Maternal Depression and Anxiety Symptoms with Infant White Matter Microstructure. JAMA Pediatr. 2018;172(10):973–981. doi:10.1001/jamapediatrics.2018.2132.
30.
Qiu A, Rifkin-Graboi A, Chen H, et al. Maternal anxiety and infants’ hippocampal development: timing matters. Transl Psychiatry. 2013;3(9):306–7. doi:10.1038/tp.2013.79.
31.
Ververs T, Van Dijk L, Yousofi S, Schobben F, Ha Visser G. Depression during pregnancy: Views on antidepressant use and information sources of general practitioners and pharmacists. BMC Health Serv Res. 2009;9:1–9. doi:10.1186/1472-6963-9-119.
32.
Folliard KJ, Crozier K, Wadnerkar Kamble MM. “Crippling and unfamiliar”: Analysing the concept of perinatal anxiety; definition, recognition and implications for psychological care provision for women during pregnancy and early motherhood. J Clin Nurs. 2020;29(23–24):4454–4468. doi:10.1111/jocn.15497.
33.
Phillips L. Assessing the knowledge of perinatal mental illness among student midwives. Nurse Educ Pract. 2015;15(6):463–469. doi:10.1016/j.nepr.2014.09.003.
34.
McGookin A, Furber C, Smith DM. Student midwives’ awareness, knowledge, and experiences of antenatal anxiety within clinical practice. J Reprod Infant Psychol. 2017;35(4):380–393. doi:10.1080/02646838.2017.1337270.
35.
Carroll M, Downes C, Gill A, et al. Knowledge, confidence, skills and practices among midwives in the republic of Ireland in relation to perinatal mental health care: The mind mothers study. Midwifery. 2018;64:29–37. doi:10.1016/j.midw.2018.05.006.
36.
Coleman VH, Carter MM, Morgan MA, Schulkin J. Obstetrician-gynecologists’ screening patterns for anxiety during pregnancy. Depress Anxiety. 2008;25(2):114–123. doi:10.1002/da.20278.
37.
Míguez MC, Vázquez MB. Prevalence of depression during pregnancy in spanish women: Trajectory and risk factors in each trimester. Int J Environ Res Public Health. 2021;18(13). doi:10.3390/ijerph18136789.
38.
Tomfohr-Madsen LM, Racine N, Giesbrecht GF, Lebel C, Madigan S. Depression and anxiety in pregnancy during COVID-19: A rapid review and meta-analysis. Psychiatry Res. 2021;300(12):113912. doi:10.1016/j.psychres.2021.113912.
39.
Abdelhai R, Mosleh H. Screening for antepartum anxiety and depression and their association with domestic violence among Egyptian pregnant women. J Egypt Public Health Assoc. 2015;90(3):101–108. doi:10.1097/01.EPX.0000471670.64665.8f.
40.
Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. doi:10.1016/S0140-6736(15)60692-4.
41.
McCauley M, Brown A, Ofosu B, Van Den Broek N. “I just wish it becomes part of routine care”: Healthcare providers’ knowledge, attitudes and perceptions of screening for maternal mental health during and after pregnancy: A qualitative study. BMC Psychiatry. 2019;19:279 DOI: 10.1186/s. BMC Psychiatry. 2019;19(1):1–8. doi:10.1186/s12888-019-2295-0.
42.
Rallis S, Skouteris H, McCabe M, Milgrom J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women and Birth. 2014;27(4):36–42. doi:10.1016/j.wombi.2014.08.002.
43.
Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in Northern Tanzania: A cross-sectional study. BMC Womens Health. 2015;15(1):1–10. doi:10.1186/s12905-015-0225-y.
44.
Hakanen H, Flykt M, Sinervä E, et al. How maternal pre- and postnatal symptoms of depression and anxiety affect early mother-infant interaction? J Affect Disord. 2019;257(4):83–90. doi:10.1016/j.jad.2019.06.048.
45.
Huizink AC, Menting B, Oosterman M, Verhage ML, Kunseler FC, Schuengel C. The interrelationship between pregnancy-specific anxiety and general anxiety across pregnancy: A longitudinal study. J Psychosom Obstet Gynecol. 2014;35(3):92–100. doi:10.3109/0167482X.2014.944498.
46.
Coleman VH, Carter MM, Morgan MA, Schulkin J. United States obstetrician-gynecologists’ accuracy in the simulation of diagnosing anxiety disorders and depression during pregnancy. J Psychosom Obstet Gynecol. 2008;29(3):177–188. doi:10.1080/01674820701833265.
47.
Weinreb L, Byatt N, Moore Simas TA, Tenner K, Savageau JA. What happens to mental health treatment during pregnancy? Women’s experience with prescribing providers. Psychiatr Q. 2014;85(3):349–355. doi:10.1007/s11126-014-9293-7.
48.
Easter A, Howard LM, Sandall J. Recognition and response to life-threatening situations among women with perinatal mental illness: A qualitative study. BMJ Open. 2019;9(3):1–8. doi:10.1136/bmjopen-2018-025872.
49.
Smith T, Gemmill AW, Milgrom J. Perinatal anxiety and depression: Awareness and attitudes in Australia. Int J Soc Psychiatry. 2019;65(5):378–387. doi:10.1177/0020764019852656.
50.
Wisner KL, Sit DKY, McShea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–498. doi:10.1001/jamapsychiatry.2013.87.
51.
Patabendige M, Athulathmudali SR, Chandrasinghe SK. Mental Health Problems during Pregnancy and the Postpartum Period: A Multicenter Knowledge Assessment Survey among Healthcare Providers. J Pregnancy. 2020;2020. doi:10.1155/2020/4926702.
52.
Gawley L, Einarson A, Bowen A. Stigma and attitudes towards antenatal depression and antidepressant use during pregnancy in healthcare students. Adv Heal Sci Educ. 2011;16(5):669–679. doi:10.1007/s10459-011-9289-0.
53.
Evans K, Spiby H, Morrell CJ. A psychometric systematic review of self-report instruments to identify anxiety in pregnancy. J Adv Nurs. 2015;71(9):1986–2001. doi:10.1111/jan.12649.
54.
Brunton RJ, Dryer R, Krägeloh C, Saliba A, Kohlhoff J, Medvedev O. The pregnancy-related anxiety scale: A validity examination using Rasch analysis. J Affect Disord. 2018;236:127–135. doi:10.1016/j.jad.2018.04.116.
55.
Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–2192. doi:10.1016/S0140-6736(16)31472-6.
56.
Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth. 2006;33(4):323–331. doi:10.1111/j.1523-536X.2006.00130.x.
57.
Huizink AC, Delforterie MJ, Scheinin NM, Tolvanen M, Karlsson L, Karlsson H. Adaption of pregnancy anxiety questionnaire–revised for all pregnant women regardless of parity: PRAQ-R2. Arch Womens Ment Health. 2016;19(1):125–132. doi:10.1007/s00737-015-0531-2.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.