Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
Editor's Choice
RESEARCH PAPER
Safety and Utility of Increased Doses of Nadroparin during Extracorporeal Membrane Oxygenation
in Respiratory Failure
1
Marta Szczukocka, II Department of Anesthesiology
and Intensive Care, Medical University, Lublin, Poland
Corresponding author
Marta Szczukocka
II Department of Anesthesiology and Intensive Care, Medical University of Lublin, Lublin, Poland., Stanisława Staszica 16, 20-081, Lublin, Poland
II Department of Anesthesiology and Intensive Care, Medical University of Lublin, Lublin, Poland., Stanisława Staszica 16, 20-081, Lublin, Poland
J Pre Clin Clin Res. 2024;18(2):98-102
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Continuous monitoring of coagulation is essential during venovenous Extracorporeal Membrane Oxygenation (VV ECMO) therapy because the extracorporeal circuit can activate the coagulation system and may lead to clot formation or bleeding. Various anticoagulant agents are used for this purpose, and unfractionated heparin is considered the gold standard of anticoagulant therapy. The biocompatibility of the extracorporeal circuit also allows antithrombotic treatment with low molecular weight heparins (LMWHs) administered subcutaneously (s.c.). There is increasing evidence that the use of LMWHs produces identical therapeutic effects with fewer side-effects. Our primary aim was to compare thrombotic complications and bleeding events.
Material and methods:
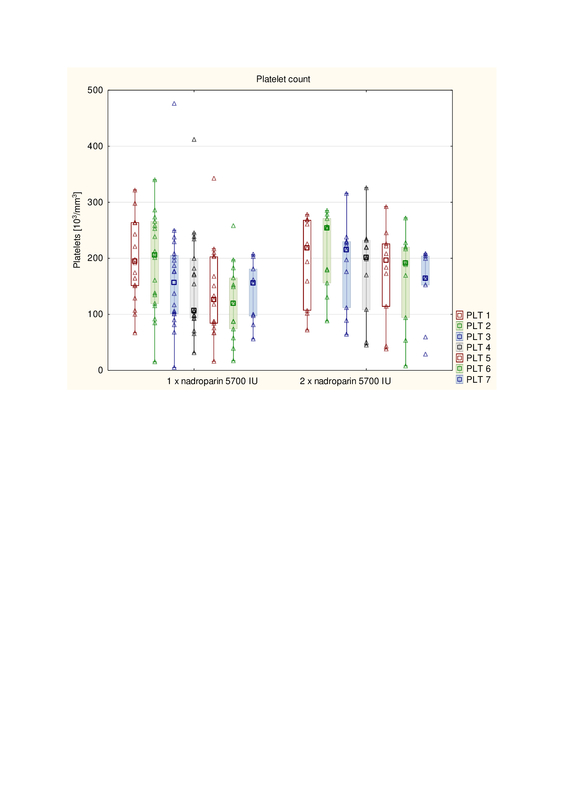
The study evaluated the safety and efficacy of anticoagulation with single-dose nadroparin administered s.c., compared with a twice daily regime of this LMWH during ECMO therapy in patients with severe respiratory failure treated in an intensive care unit (ICU). Changes in flow resistance in the oxygenator and the number of transfused blood products were monitored. No differences were found in bleeding events between once and twice-daily dosing of nadroparin during ECMO therapy (34% vs. 53%, p = 12).
Results:
Both regimes of administration were similar in the number of life-threatening bleeding events (p =.26) and a daily number of transfused red blood cells (p =.37). The change in flow resistance in the oxygenator was comparable between the two groups (11.28% vs. 6.13%, respectively, p = .26).
Conclusions:
Once daily administration of nadroparin appeared comparable to the twice daily regime in terms of the number of thrombotic complications.
Continuous monitoring of coagulation is essential during venovenous Extracorporeal Membrane Oxygenation (VV ECMO) therapy because the extracorporeal circuit can activate the coagulation system and may lead to clot formation or bleeding. Various anticoagulant agents are used for this purpose, and unfractionated heparin is considered the gold standard of anticoagulant therapy. The biocompatibility of the extracorporeal circuit also allows antithrombotic treatment with low molecular weight heparins (LMWHs) administered subcutaneously (s.c.). There is increasing evidence that the use of LMWHs produces identical therapeutic effects with fewer side-effects. Our primary aim was to compare thrombotic complications and bleeding events.
Material and methods:
The study evaluated the safety and efficacy of anticoagulation with single-dose nadroparin administered s.c., compared with a twice daily regime of this LMWH during ECMO therapy in patients with severe respiratory failure treated in an intensive care unit (ICU). Changes in flow resistance in the oxygenator and the number of transfused blood products were monitored. No differences were found in bleeding events between once and twice-daily dosing of nadroparin during ECMO therapy (34% vs. 53%, p = 12).
Results:
Both regimes of administration were similar in the number of life-threatening bleeding events (p =.26) and a daily number of transfused red blood cells (p =.37). The change in flow resistance in the oxygenator was comparable between the two groups (11.28% vs. 6.13%, respectively, p = .26).
Conclusions:
Once daily administration of nadroparin appeared comparable to the twice daily regime in terms of the number of thrombotic complications.
Szczukocka M. Safety and Utility of Increased doses of Nadroparin during Extracorporeal Membrane Oxygenation in Respiratory Failure.
J Pre-Clin Clin Res. 2024; 18(2): 98–102. doi: 10.26444/jpccr/186747
REFERENCES (19)
1.
Burrell A, Kim J, Alliegro P, Romero L, Serpa Neto A, Mariajoseph F, Hodgson C. Extracorporeal membrane oxygenation for critically ill adults. Cochrane Database Syst Rev. 2023;9(9):CD010381. https://doi.org/10.1002/146518....
2.
Munshi L, Walkey A, Goligher E, Pham T, Uleryk EM, Fan E. Venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis. Lancet Respir Med. 2019;7(2):163–172. https://doi.org/10.1016/S2213-....
3.
Aubron C, Cheng AC, Pilcher D, Leong T, Magrin G, Cooper DJ, Scheinkestel C, Pellegrino V. Factors associated with outcomes of patients on extracorporeal membrane oxygenation support: a 5-year cohort study. Crit Care. 2013;17(2):R73. https://doi.org/10.1186/cc1268....
4.
Raghunathan V, Liu P, Kohs TCL, Amirsoltani R, Oakes M, McCarty OJT, Olson SR, Zonies D, Shatzel JJ. Heparin Resistance Is Common in Patients Undergoing Extracorporeal Membrane Oxygenation but Is Not Associated with Worse Clinical Outcomes. ASAIO J. 2021;67:899–906. https://doi.org/10.1097/MAT.00....
5.
Bridges B, Ranucci M, Lequier L, Anticoagulation and Disorders of Hemostasis. In: Brogan T, Lequier L, Lorusso R, et al, editors. Extracorporeal Life Support The ELSO Red Book. 2017. Red Book 5th ed. Ann Arbor, MI: Extracorporeal Life Support Organization; p. 93–99.
6.
Teijeiro-Paradis R, Gannon WD, Fan E. Complications Associated With Venovenous Extracorporeal Membrane Oxygenation-What Can Go Wrong? Crit Care Med. 2022;50(12):1809–1818. https://doi.org/10.1097/CCM.00....
7.
Nunez JI, Gosling AF, O’Gara B, Kennedy KF, Rycus P, Abrams D, Brodie D, Shaefi S, Garan AR, Grandin EW. Bleeding and thrombotic events in adults supported with venovenous extracorporeal membrane oxygenation: an ELSO registry analysis. Intensive Care Med. 2022;48(2):213–224. https://doi.org/10.1007/s00134....
8.
Martucci G, Schmidt M, Agerstrand C, Tabatabai A, Tuzzolino F, Giani M, Ramanan R, Grasselli G, Schellongowski P, Riera J, Hssain AA, Duburcq T, Gorjup V, De Pascale G, Buabbas S, Gannon WD, Jeon K, Trethowan B, Fanelli V, Chico JI, Balik M, Broman LM, Pesenti A, Combes A, Ranieri MV, Foti G, Buscher H, Tanaka K, Lorusso R, Arcadipane A, Brodie D; International ECMO Network (ECMONet). Transfusion practice in patients receiving VV ECMO (PROTECMO): a prospective, multicentre, observational study. Lancet Respir Med. 2023;11(3):245–255. https://doi.org/10.1016/S2213-....
9.
Piwowarczyk P, Borys M, Kutnik P, Szczukocka M, Sysiak-Sławecka J, Szułdrzyński K, Ligowski M, Drobiński D, Czarnik T, Czuczwar M. Unfractionated Heparin Versus Subcutaneous Nadroparin in Adults Supported With Venovenous Extracorporeal Membrane Oxygenation: a Retrospective, Multicenter Study. ASAIO J. 2021;67(1):104–111. https://doi.org/10.1097/MAT.00....
10.
Geli J, Capoccia M, Maybauer DM, Maybauer MO. Argatroban Anticoagulation for Adult Extracorporeal Membrane Oxygenation: A Systematic Review. J Intensive Care Med. 2022;37(4):459–471. https://doi.org/10.1177/088506....
11.
Stattin K, Lipcsey M, Andersson H, Pontén E, Bülow Anderberg S, Gradin A, Larsson A, Lubenow N, von Seth M, Rubertsson S, Hultström M, Frithiof R. Inadequate prophylactic effect of low-molecular weight heparin in critically ill COVID-19 patients. J Crit Care. 2020;60:249–252. https://doi.org/10.1016/j.jcrc....
12.
Piagnerelli M, Cauchie P, Vancutsem M, Thooft A, Zouaoui Boudjeltia K, Biston P, Wautrecht JC. Thromboprophylaxis in Critically Ill Coronavirus Disease 2019 Patients. Crit Care Explor. 2020;2(8):e0177. https://doi.org/10.1097/CCE.00....
13.
Lubnow M, Philipp A, Foltan M, et al. Technical complications during veno-venous extracorporeal membrane oxygenation and their relevance predicting a system-exchange–retrospective analysis of 265 cases. PLoS One. 2014;9:e112316. https://doi.org/10.1371/journa....
14.
Krueger K, Schmutz A, Zieger B, Kalbhenn J. Venovenous Extracorporeal Membrane Oxygenation With Prophylactic Subcutaneous Anticoagulation Only: An Observational Study in More Than 60 Patients. Artif Organs. 2017;41(2):186–192. https://doi.org/10.1111/aor.12....
15.
Gratz J, Pausch A, Schaden E, Baierl A, Jaksch P, Erhart F, Hoetzenecker K, Wiegele M. Low molecular weight heparin versus unfractioned heparin for anticoagulation during perioperative extracorporeal membrane oxygenation: A single center experience in 102 lung transplant patients. Artif Organs. 2020;44(6):638–646. https://doi.org/10.1111/aor.13....
16.
Shah A, Donovan K, McHugh A, Pandey M, Aaron L, Bradbury CA, Stanworth SJ, Alikhan R, Von Kier S, Maher K, Curry N, Shapiro S, Rowland MJ, Thomas M, Mason R, Holland M, Holmes T, Ware M, Gurney S, McKechnie SR. Thrombotic and haemorrhagic complications in critically ill patients with COVID-19: a multicentre observational study. Crit Care. 2020;24(1):561. https://doi.org/10.1186/s13054....
17.
Dibiasi C, Gratz J, Wiegele M, Baierl A, Schaden E. Anti-factor Xa Activity Is Not Associated With Venous Thromboembolism in Critically Ill Patients Receiving Enoxaparin for Thromboprophylaxis: A Retrospective Observational Study. Front Med (Lausanne). 2022;9:7 https://doi.org/10.3389/fmed.2....
18.
Piwowarczyk P, Szczukocka M, Cios W, Okuńska P, Raszewski G, Borys M, Wiczling P, Czuczwar M. Population Pharmacokinetics and Probability of Target Attainment Analysis of Nadroparin in Different Stages of COVID-19. Clin Pharmacokinet. 2023; 62(6):835–847. https://doi.org/10.1007/s40262....
19.
Circelli A, Velia Antonini M, Gamberini E, Bissoni L, Scognamiglio G, Viola L, Agnoletti V; ECMO Team of the Anesthesia and Intensive Care Unit, Bufalini Hospital—AUSL della Romagna. Anticoagulation on Extracorporeal Support: An Alternative Strategy. ASAIO J. 2023;69:e131. https://doi.org/10.1097/MAT.00....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.