Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Risk factors for carpal tunnel syndrome
1
Department of Clinical Interventional Sciences, University of Technology and Humanities Casimir Pulaski, Radom, Poland
Corresponding author
Bartłomiej Kulesza
Department of Clinical Interventional Sciences, University of Technology and Humanities Casimir Pulaski, Radom, Poland
Department of Clinical Interventional Sciences, University of Technology and Humanities Casimir Pulaski, Radom, Poland
J Pre Clin Clin Res. 2023;17(3):167-170
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Carpal tunnel syndrome (CTS) is a common condition characterized by the compression of the median nerve in the wrist. Left untreated, it leads to significant discomfort and loss of motor function in the hand. The aim of this systematic review is to identify and evaluate recent research on risk factors associated with CTS.
Review methods:
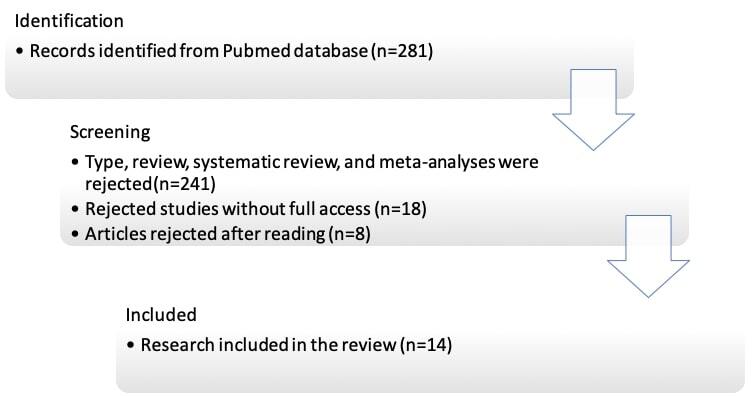
A systematic search of the PubMed/MEDLINE database was conducted, focusing on studies published within the last 5 years. The search strategy used relevant key words related to CTS and risk factors. Studies were included if they provided information on risk factors associated with CTS in the adult population. Review articles, systematic reviews and meta-analyses were excluded.
Brief description of the state of knowledge:
Risk factors for CTS include repetitive hand movements in occupations that require typing, certain anatomical and physiological characteristics (e.g., smaller carpal tunnel size), age (risk increases with age), gender (higher risk in women), pregnancy, medical conditions (e.g., obesity, diabetes, arthritis, metabolic syndrome), and previous trauma or injury to the wrist. On-going research continues to shed light on the subject
Summary:
The systematic review found that physical labour, working in pain, and certain co-morbidities were strongly associated with an increased risk of developing CTS. Occupations such as grocery store workers, hairdressers, telephone operators and manual labourers (blue-collar workers) showed a significant association with the development of CTS, compared to the general population. Further studies are needed to investigate the potential impact of bilateral ovarian resection and alcohol consumption as risk factors. These findings underscore the importance of considering occupational factors and co-morbidities when assessing the risk of CTS.
Carpal tunnel syndrome (CTS) is a common condition characterized by the compression of the median nerve in the wrist. Left untreated, it leads to significant discomfort and loss of motor function in the hand. The aim of this systematic review is to identify and evaluate recent research on risk factors associated with CTS.
Review methods:
A systematic search of the PubMed/MEDLINE database was conducted, focusing on studies published within the last 5 years. The search strategy used relevant key words related to CTS and risk factors. Studies were included if they provided information on risk factors associated with CTS in the adult population. Review articles, systematic reviews and meta-analyses were excluded.
Brief description of the state of knowledge:
Risk factors for CTS include repetitive hand movements in occupations that require typing, certain anatomical and physiological characteristics (e.g., smaller carpal tunnel size), age (risk increases with age), gender (higher risk in women), pregnancy, medical conditions (e.g., obesity, diabetes, arthritis, metabolic syndrome), and previous trauma or injury to the wrist. On-going research continues to shed light on the subject
Summary:
The systematic review found that physical labour, working in pain, and certain co-morbidities were strongly associated with an increased risk of developing CTS. Occupations such as grocery store workers, hairdressers, telephone operators and manual labourers (blue-collar workers) showed a significant association with the development of CTS, compared to the general population. Further studies are needed to investigate the potential impact of bilateral ovarian resection and alcohol consumption as risk factors. These findings underscore the importance of considering occupational factors and co-morbidities when assessing the risk of CTS.
Nowak W, Znamirowska P, Szmigielska N, Zemsta K, Miśkiewicz J, Plata H, Pałatyńska M, Kulesza B. Risk factors for carpal tunnel syndrome.
J Pre-Clin Clin Res. 2023; 17(3): 167–170. doi: 10.26444/jpccr/168559
REFERENCES (20)
1.
Sevy JO, Varacallo M. Carpal Tunnel Syndrome. 2022 Sep 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. PMID: 28846321.
2.
Burton C, Chesterton LS, Davenport G. Diagnosing and managing carpal tunnel syndrome in primary care. Br J Gen Pract. 2014 May;64(622):262–3. doi:10.3399/bjgp14X679903. PMID: 24771836; PMCID: PMC4001168.
3.
Genova A, Dix O, Saefan A, Thakur M, Hassan A. Carpal Tunnel Syndrome: A Review of Literature. Cureus. 2020 Mar 19;12(3):e7333. doi:10.7759/cureus.7333. PMID: 32313774; PMCID: PMC7164699.
4.
Jiménez Del Barrio S, Bueno Gracia E, Hidalgo García C, Estébanez de Miguel E, Tricás Moreno JM, Rodríguez Marco S, et al. Conservative treatment in patients with mild to moderate carpal tunnel syndrome: A systematic review. Neurologia (Engl Ed). 2018 Nov-Dec;33(9):590–601. English, Spanish. doi:10.1016/j.nrl.2016.05.018. Epub 2016 Jul 22. PMID: 27461181.
5.
Wipperman J, Goerl K. Carpal Tunnel Syndrome: Diagnosis and Management. Am Fam Physician. 2016 Dec 15;94(12):993–999. PMID: 28075090.
6.
Petrover D, Richette P. Treatment of carpal tunnel syndrome: from ultrasonography to ultrasound guided carpal tunnel release. Joint Bone Spine. 2018 Oct;85(5):545–552. doi:10.1016/j.jbspin.2017.11.003. Epub 2017 Nov 16. PMID: 29154980.
7.
Cardona A, Thiese MS, Kapellusch J, Merryweather A, Wood E, Hegmann KT. Role of Biomechanical Factors in Resolution of Carpal Tunnel Syndrome Among a Population of Workers. J Occup Environ Med. 2019 Apr;61(4):340–346. doi:10.1097/JOM.0000000000001558. PMID: 30789447; PMCID: PMC6449203.
8.
Möllestam K, Englund M, Atroshi I. Association of clinically relevant carpal tunnel syndrome with type of work and level of education: a general-population study. Sci Rep. 2021;11(1):19850. Published 2021 Oct 6. doi:10.1038/s41598-021-99242-8.
9.
Jackson R, Beckman J, Frederick M, Musolin K, Harrison R. Rates of Carpal Tunnel Syndrome in a State Workers’ Compensation Information System, by Industry and Occupation – California, 2007–2014. MMWR Morb Mortal Wkly Rep. 2018;67(39):1094–1097. Published 2018 Oct 5. doi:10.15585/mmwr.mm6739a4.
10.
Feng B, Chen K, Zhu X, Ip WY, Andersen LL, Page P, et al. Prevalence and risk factors of self-reported wrist and hand symptoms and clinically confirmed carpal tunnel syndrome among office workers in China: a cross-sectional study. BMC Public Health. 2021 Jan 6;21(1):57. doi:10.1186/s12889-020-10137-1. PMID: 33407293; PMCID: PMC7789363.
11.
Erick P, Benjamin K, Raditloko S, Tapera R, Mbongwe B. Risk factors for self-reported carpal tunnel syndrome among hairstylists in Gaborone, Botswana. Int J Occup Med Environ Health. 2021 Jun 28;34(3):437–450. doi:10.13075/ijomeh.1896.01659. Epub 2020 Dec 29. PMID: 33399136.
12.
Wiberg A, Smillie RW, Dupré S, Schmid AB, Bennett DL, Furniss D. Replication of epidemiological associations of carpal tunnel syndrome in a UK population-based cohort of over 400,000 people. J Plast Reconstr Aesthet Surg. 2022 Mar;75(3):1034–1040. doi:10.1016/j.bjps.2021.11.025. Epub 2021 Nov 14. PMID: 34916160; PMCID: PMC8982328.
13.
Pourmemari MH, Heliövaara M, Viikari-Juntura E, Shiri R. Carpal tunnel release: Lifetime prevalence, annual incidence, and risk factors. Muscle Nerve. 2018 Oct;58(4):497–502. doi:10.1002/mus.26145. Epub 2018 May 18. PMID: 29665085.
14.
Sharief F, Kanmani J, Kumar S. Risk factors, symptom severity and functional status among patients with carpel tunnel syndrome. Neurol India. 2018 May-Jun;66(3):743–746. doi:10.4103/0028-3886.232351. PMID: 29766936.
15.
Ulbrichtová R, Jakušová V, Osina O, Zibolenová J, Kuka S, Hudečková H. Association of the role of personal variables and nonoccupational risk factors for work-related carpal tunnel syndrome. Cent Eur J Public Health. 2020 Dec;28(4):274–278. doi:10.21101/cejph.a6109. PMID: 33338362.
16.
Trybus M, Stepańczak B, Koziej M, Gniadek M, Kołodziej M, Hołda MK. Hand anthropometry in patients with carpal tunnel syndrome: a case-control study with a matched control group of healthy volunteers. Folia Morphol (Warsz). 2019;78(1):182–190. doi:10.5603/FM.a2018.0049. Epub 2018 May 26. PMID: 29802717.
17.
Leow JM, Clement ND, McQueen MM, Duckworth AD. The rate and associated risk factors for acute carpal tunnel syndrome complicating a fracture of the distal radius. Eur J Orthop Surg Traumatol. 2021 Jul;31(5):981–987. doi:10.1007/s00590-021-02975-5. Epub 2021 Apr 23. PMID: 33891155; PMCID: PMC8233234.
18.
Wang JS, Chen WS, Lin CL, Wang IK, Shen MY. Risk of carpal tunnel syndrome after parathyroidectomy in patients with end-stage renal disease: A population-based cohort study in Taiwan. Medicine (Baltimore). 2020;99(20):e20313. doi:10.1097/MD.0000000000020313.
19.
Yeh KT, Lee RP, Yu TC, Wang JH, Liu KL, Peng CH, et al. Risk factors for carpal tunnel syndrome or trigger finger following distal radius fracture: a nationwide study. Sci Rep. 2020 Jan 16;10(1):469. doi:10.1038/s41598-020-57415-x. PMID: 31949231; PMCID: PMC6965085.
20.
Starlinger J, Schrier VJMM, Smith CY, Song J, Stewart EA, Gazzuola Rocca L, et al. Risk of de novo severe carpal tunnel syndrome after bilateral oophorectomy: a population-based cohort study. Menopause. 2021 May 24;28(9):1026–1036. doi:10.1097/GME.0000000000001804. PMID: 34033605; PMCID: PMC8403136.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.