Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Primary healthcare antibiotic therapy in Poland: a patient perspective – preliminary survey study
1
Department of Clinical Pharmacy and Biopharmacy, Poznan University of Medical Sciences, Poznan, Poland
2
Doctoral School, Poznan University of Medical Sciences, Poznan, Poland
3
SciencePharma, Warsaw, Poland
4
Department of Clinical Pharmacology, Wroclaw Medical University, Wroclaw, Poland
5
Clinical Pharmacy Team, Jan Mikulicz-Radecki University Teaching Hospital, Wroclaw, Poland
Corresponding author
Arkadiusz Mateusz Adamiszak
Department of Clinical Pharmacy, Poznan University of Medical Sciences, Rokietnicka 3, 60-806, Poznań, Poland
Department of Clinical Pharmacy, Poznan University of Medical Sciences, Rokietnicka 3, 60-806, Poznań, Poland
J Pre Clin Clin Res. 2023;17(3):176-181
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Growing resistance to commonly used antibiotics has challenged 21st-century medicine. To date, antibiotic policy has induced bacterial resistance and isolation of multi-drug resistant superbugs insensitive to known antibiotics. The aim of the study was to investigate the knowledge of primary healthcare patients about antibiotic usage, and to identify incorrect patient habits.
Material and methods:
The research was based on a proprietary, anonymous Internet survey consisting of 21 questions, in which only adults could participate. The survey selected nine questions to assess the respondents’ knowledge.
Results:
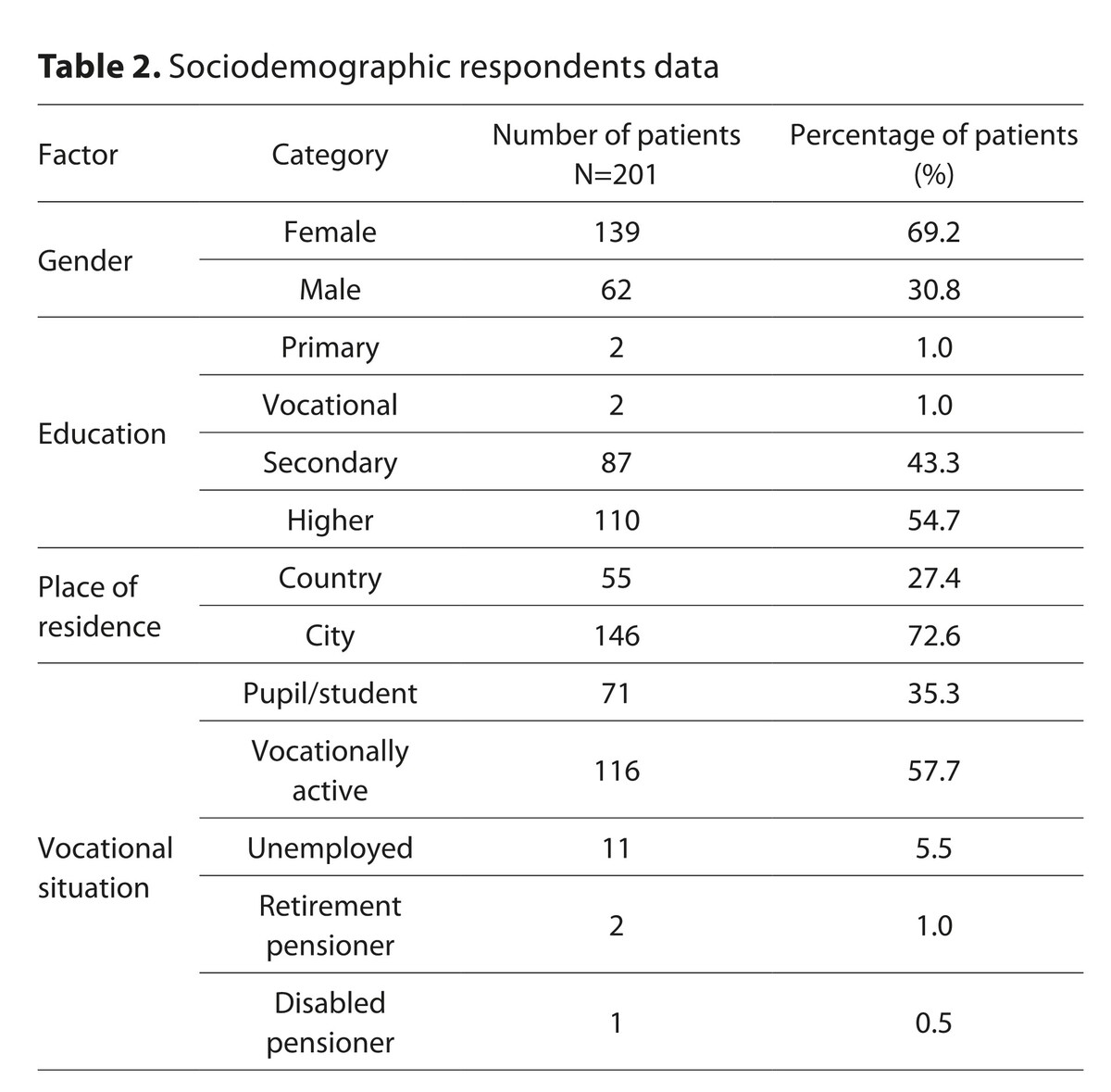
201 patients participated in the study. About 50% of participants based their knowledge about antibiotics on information obtained during a medical visit, 16.4% on consultations with a pharmacist, 24.9% on the Internet, and 11.4% exchanged experiences with friends. Every third respondent was not satisfied with the information obtained from a doctor. People with higher education reported this issue more often (p<0.05). Nearly 35% of people living in the countryside (p<0.05) admitted to using the part of a drug left after previous antibiotic therapy, and 10% administered antibiotics obtained from friends or relatives. Every fourth patient believed that antibiotics were effective against colds and flu. The average knowledge test result was 5.49 out of 9 points, and a positive score of 6 or more was obtained by nearly 60% of the respondents.
Conclusions:
The results of this preliminary study indicate that more focus should be given to improving patients’ education and compliance with treatment recommendations.
Growing resistance to commonly used antibiotics has challenged 21st-century medicine. To date, antibiotic policy has induced bacterial resistance and isolation of multi-drug resistant superbugs insensitive to known antibiotics. The aim of the study was to investigate the knowledge of primary healthcare patients about antibiotic usage, and to identify incorrect patient habits.
Material and methods:
The research was based on a proprietary, anonymous Internet survey consisting of 21 questions, in which only adults could participate. The survey selected nine questions to assess the respondents’ knowledge.
Results:
201 patients participated in the study. About 50% of participants based their knowledge about antibiotics on information obtained during a medical visit, 16.4% on consultations with a pharmacist, 24.9% on the Internet, and 11.4% exchanged experiences with friends. Every third respondent was not satisfied with the information obtained from a doctor. People with higher education reported this issue more often (p<0.05). Nearly 35% of people living in the countryside (p<0.05) admitted to using the part of a drug left after previous antibiotic therapy, and 10% administered antibiotics obtained from friends or relatives. Every fourth patient believed that antibiotics were effective against colds and flu. The average knowledge test result was 5.49 out of 9 points, and a positive score of 6 or more was obtained by nearly 60% of the respondents.
Conclusions:
The results of this preliminary study indicate that more focus should be given to improving patients’ education and compliance with treatment recommendations.
Adamiszak A, Adamiszak S, Dobrek Ł, Fedorowicz O, Bienert A. Primary healthcare antibiotic therapy in Poland – a preliminary survey. J
Pre-Clin Clin Res. 2023; 17(3): 176–181. doi: 10.26444/jpccr/169613
REFERENCES (31)
1.
Hashiguchi TCO, Ouakrim DA, Padget M, et al. Resistance proportions for eight priority antibiotic-bacterium combinations in OECD, EU/EEA and G20 countries 2000 to 2030: A modelling study. Eurosurveillance. 2019;24(20):1. doi:10.2807/1560-7917.ES.2019.24.20.1800445.
2.
Zawodzą antybiotyki ostatniego rzutu – Publications Office of the EU. Accessed September 22, 2022. https://op.europa.eu/pl/public....
3.
McCullough AR, Parekh S, Rathbone J, et al. A systematic review of the public’s knowledge and beliefs about antibiotic resistance. Journal of Antimicrobial Chemotherapy. 2016;71(1):27–33. doi:10.1093/jac/dkv310.
4.
Benmerzouga I, Al-Zammay SA, Al-Shammari MM, et al. Practices of patients consuming antibiotics and knowledge about antibiotic resistance in Hail region – Saudi Arabia. Future Sci OA. 2019;5(10). doi:10.2144/fsoa-2019-0054.
5.
Sundvall PD, Skoglund I, Hess-Wargbaner M, et al. Rational antibiotic prescribing in primary care: qualitative study of opportunities and obstacles. BJGP Open. 2020;4(4):1–10. doi:10.3399/BJGPOPEN20X101079.
6.
Mason T, Trochez C, Thomas R, et al. Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance. BMC Public Health. 2018;18(1):1–10. doi:10.1186/s12889-018-5614-3.
7.
Antimicrobial consumption in the EU/EEA (ESAC-Net) – Annual Epidemiological Report for 2021. Accessed July 10, 2023. https://www.ecdc.europa.eu/en/....
8.
D’Atri F, Arthur J, Blix HS, et al. Targets for the reduction of antibiotic use in humans in the Transatlantic Taskforce on Antimicrobial Resistance (TATFAR) partner countries. Eurosurveillance. 2019;24(28). doi:10.2807/1560-7917.ES.2019.24.28.1800339.
9.
Chiswell E, Hampton D, Okoli CTC. Effect of Patient and Provider Education on Antibiotic Overuse for Respiratory Tract Infections. J Healthc Qual. 2019;41(3):E13-E20. doi:10.1097/JHQ.0000000000000144.
10.
Fallatah MS, Alzahrani AA, Alghamdi GS, et al. Patient Beliefs on Antibiotic Prescribing in Primary Care: A Cross-Sectional Survey in Saudi Arabia. Cureus. 2023;15(4). doi:10.7759/CUREUS.38254.
11.
Hemkens LG, Saccilotto R, Reyes SL, et al. Personalized prescription feedback to reduce antibiotic overuse in primary care: rationale and design of a nationwide pragmatic randomized trial. BMC Infect Dis. 2016;16(1). doi:10.1186/S12879-016-1739-0.
12.
Łoś-Rycharska E, Czerwionka-Szaflarska M. Antybiotykoterapia w Polsce – zwyczaje preskrypcyjne a rekomendacje. Pediatr Pol. 2016;91(1):1–6. doi:10.1016/j.pepo.2015.09.002.
13.
Glinz D, Mc Cord KA, Moffa G, et al. Antibiotic prescription monitoring and feedback in primary care in Switzerland: Design and rationale of a nationwide pragmatic randomized controlled trial. Contemp Clin Trials Commun. 2021;21. doi:10.1016/J.CONCTC.2021.100712.
14.
Napolitano F, Izzo MT, Di Giuseppe G, et al. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8(12). doi:10.1371/journal.pone.0084177.
15.
WHO. World Antimicrobial Awareness Week. World Antimicrobial Awareness Week 2021. Published 2021. Accessed July 6, 2022. https://www.who.int/campaigns/....
16.
Sprawozdanie z realizacji w Polsce Kampanii “Europejski Dzień Wiedzy o Antybiotykach ‘2020.” Published online 2021. Accessed July 6, 2022. https://antybiotyki.edu.pl/edw....
17.
Pavyde E, Veikutis V, Mačiuliene A, Mačiulis V, Petrikonis K, Stankevičius E. Public knowledge, beliefs and behavior on antibiotic use and self-medication in Lithuania. Int J Environ Res Public Health. 2015;12(6):7002–7016. doi:10.3390/ijerph120607002.
18.
Special Eurobarometer 478 Special Eurobarometer 478-Wave EB90.1-Kantar Public Brussels Antimicrobial Resistance Report Fieldwork. Published online 2018. Accessed September 16, 2022. doi:10.2875/92205.
19.
Robert A, Nguyen Y, Bajolet O, et al. Facteurs associés a la connaissance des antibiotiques et a leur résistance chez les patients consultant en médecine générale. Med Mal Infect. 2017;47(2):142–151. doi:10.1016/j.medmal.2016.10.003.
20.
Demoré B, Mangin L, Tebano G, et al. Public knowledge and behaviours concerning antibiotic use and resistance in France: a cross-sectional survey. Infection. 2017;45(4):513–520. doi:10.1007/s15010-017-1015-2.
21.
Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS One. 2015;10(2):e0117910. doi:10.1371/journal.pone.0117910.
22.
Kim SS, Moon S, Kim EJ. Public Knowledge and Attitudes Regarding Antibiotic Use in South Korea. J Korean Acad Nurs. 2011;41(6):742. doi:10.4040/jkan.2011.41.6.742.
23.
Wun YT, Lam TP, Lam KF, et al. The public’s perspectives on antibiotic resistance and abuse among Chinese in Hong Kong. Pharmacoepidemiol Drug Saf. 2013;22(3):241–249. doi:10.1002/pds.3339.
24.
Mahmoudi H. Assessment of knowledge, attitudes, and practice regarding antibiotic self-treatment use among COVID-19 patients. GMS Hyg Infect Control. 2022;17:Doc12. doi:10.3205/DGKH000415.
25.
Beyene KA, Sheridan J, Aspden T. Prescription Medication Sharing: A Systematic Review of the Literature. Am J Public Health. 2014;104(4):e15. doi:10.2105/AJPH.2013.301823.
26.
Rather IA, Kim BC, Bajpai VK, et al. Self-medication and antibiotic resistance: Crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24(4):808. doi:10.1016/J.SJBS.2017.01.004.
27.
Kraśnicka J, Chlabicz S, Doroszkiewicz H. Wiedza pacjentów podstawowej opieki zdrowotnej w Białymstoku na temat antybiotyków stosowanych w chorobach układu oddechowego. Problemy Pielęg niarstwa. 2014;22(1):35–41.
28.
McNulty CAM, Lecky DM, Hawking MKD, et al. How much information about antibiotics do people recall after consulting in primary care? Fam Pract. 2016;33(4):395–400. doi:10.1093/fampra/cmw022.
29.
Guo Q, Goldenberg JZ, Humphrey C, et al. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database of Systematic Reviews. 2019;2019(4). doi:10.1002/14651858.cd004827.pub5.
30.
Draper K, Ley C, Parsonnet J. A survey of probiotic use practices among patients at a tertiary medical centre. Benef Microbes. 2017;8(3):345–351. doi:10.3920/BM2016.0148.
31.
Huh K, Chung DR, Kim SH, et al. Factors affecting the public awareness and behavior on antibiotic use. European Journal of Clinical Microbiology and Infectious Diseases. 2018;37(8):1547–1552. doi:10.1007/s10096-018-3283-x.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.