Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
Editor's Choice
REVIEW PAPER
Epilepsy diagnosis and treatment in children – new hopes and challenges – literature review
1
Students’ Scientific Association, Department of Paediatric Neurology, Medical University, Lublin, Poland
2
Department of Children’s Neurology, University Children’s Hospital, Lublin, Poland
Corresponding author
Sylwia Marta Urbańska
Students’ Scientific Association, Department of Paediatric Neurology, Medical University, Profesor Antoniego Gębali 6, 20-093 Lublin, Poland
Students’ Scientific Association, Department of Paediatric Neurology, Medical University, Profesor Antoniego Gębali 6, 20-093 Lublin, Poland
J Pre Clin Clin Res. 2024;18(1):40-49
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Epilepsy is one of the most commonly diagnosed neurological aberrations. Epileptic seizures are the main symptoms of the condition. Reducing the seizures is the main objective of the treatment. The aim of the review is to summarise current knowledge on diagnosis and various treatment methods of epilepsy among children.
Review methods:
Scientific publications in PubMed, Google Scholar, Wiley Library, Web of Science, Clinicaltrials.gov, and NCBI databases were searched for the review. More than 93% of the articles are less than eight years old. After an initial assessment of articles, meta-analyses and reviews on epilepsy, concerning the pharmacological, surgical, and gene therapy of epilepsy, were selected. Publications were analyzed using a non-systematic review method to create a brief synthesis of the information.
Brief description of the state of knowledge:
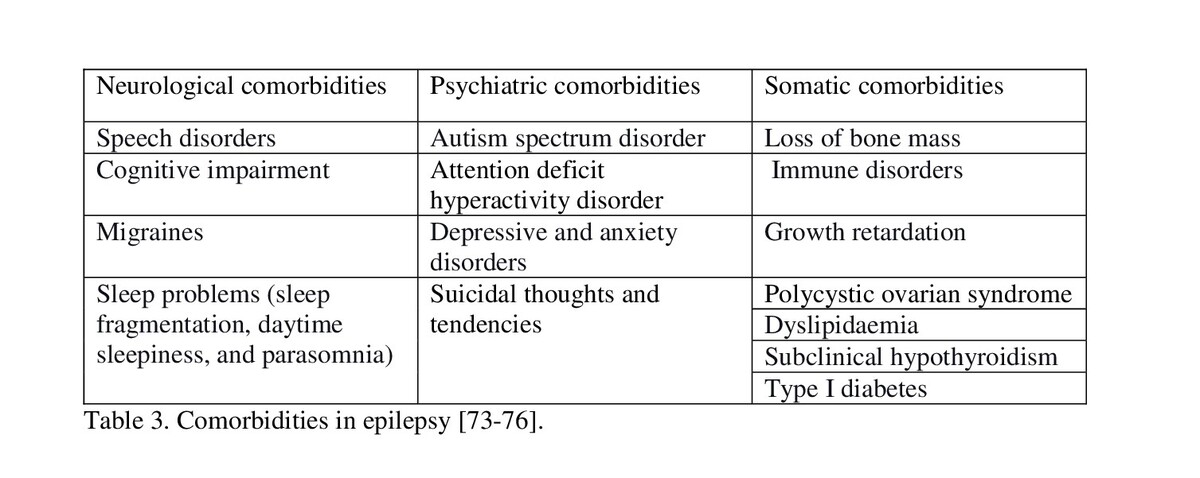
Diagnosis of epilepsy consists of subjective and objective examination of the patient and performing electroencephalography. Additional procedures, such as neuroimaging of the central nervous system, genetic testing, metabolic and immunological tests, may expand the diagnostic stage. Pharmacological methods prove that early initiation of treatment reduces the risk of relapse. First-line pharmacological treatment consists of carbamazepine, valproic acid, oxcarbazepine, and phenytoin. If epilepsy proves to be drug resistant, surgery is an alternative to pharmacotherapy. Invasive treatment consists of resection, separation and neurostimulation. Current knowledge also proves that there is relevant comorbidity among paediatric patients with epilepsy.
Summary:
The review emphasizes the development of currently used diagnostic methods, therapeutic options, and importance of further research.
Epilepsy is one of the most commonly diagnosed neurological aberrations. Epileptic seizures are the main symptoms of the condition. Reducing the seizures is the main objective of the treatment. The aim of the review is to summarise current knowledge on diagnosis and various treatment methods of epilepsy among children.
Review methods:
Scientific publications in PubMed, Google Scholar, Wiley Library, Web of Science, Clinicaltrials.gov, and NCBI databases were searched for the review. More than 93% of the articles are less than eight years old. After an initial assessment of articles, meta-analyses and reviews on epilepsy, concerning the pharmacological, surgical, and gene therapy of epilepsy, were selected. Publications were analyzed using a non-systematic review method to create a brief synthesis of the information.
Brief description of the state of knowledge:
Diagnosis of epilepsy consists of subjective and objective examination of the patient and performing electroencephalography. Additional procedures, such as neuroimaging of the central nervous system, genetic testing, metabolic and immunological tests, may expand the diagnostic stage. Pharmacological methods prove that early initiation of treatment reduces the risk of relapse. First-line pharmacological treatment consists of carbamazepine, valproic acid, oxcarbazepine, and phenytoin. If epilepsy proves to be drug resistant, surgery is an alternative to pharmacotherapy. Invasive treatment consists of resection, separation and neurostimulation. Current knowledge also proves that there is relevant comorbidity among paediatric patients with epilepsy.
Summary:
The review emphasizes the development of currently used diagnostic methods, therapeutic options, and importance of further research.
Urbańska SM, Leśniewski M, Welian-Polus I, Witas A, Szukała K, Chrościńska-Krawczyk M. Epilepsy diagnosis and treatment in children – new
hopes and challenges – literature review. J Pre-Clin Clin Res. 2024; 18(1): 40–49. doi: 10.26444/jpccr/185469
REFERENCES (93)
1.
Bastos F, Cross JH. Epilepsy. Handb Clin Neurol. 2020;174:137–158. doi:10.1016/B978-0-444-64148-9.00011-9.
2.
Falco-Walter J. Epilepsy-Definition, Classification, Pathophysiology, and Epidemiology. Semin Neurol. 2020;40(6):617–623. doi:10.1055/s-0040-1718719.
3.
Chen H, Koubeissi MZ. Electroencephalography in Epilepsy Evaluation. Continuum (Minneap Minn). 2019;25(2):431–453. doi:10.1212/CON.0000000000000705.3.
4.
Katyayan A, Diaz-Medina G. Epilepsy: Epileptic Syndromes and Treatment. Neurol Clin. 2021;39(3):779–795. doi:10.1016/j.ncl.2021.04.002.
5.
Fisher RS, Acevedo C, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–82. doi:10.1111/epi.12550.
6.
Epilepsies: diagnosis and management. London: National Institute for Health and Care Excellence (NICE); 2021 May 12. PMID: 32027473.
7.
Jiménez-Villegas MJ, Lozano-García L, Carrizosa-Moog J. Update on first unprovoked seizure in children and adults: A narrative review. Seizure. 2021;90:28–33. doi:10.1016/j.seizure.2021.03.027.
8.
Hirtz D, Ashwal S, et al. Practice parameter: evaluating a first nonfebrile seizure in children: report of the quality standards subcommittee of the American Academy of Neurology, the Child Neurology Society, and the American Epilepsy Society. Neurology. 2000;55:616–23 doi:10.1212/wnl.55.5.616.
9.
Llauradó A, Santamarina E, et al. How soon should urgent EEG be performed following a first epileptic seizure? Epilepsy Behav. 2020;111:107315. doi:10.1016/j.yebeh.2020.107315.
10.
Rozenblat T, Kraus D, et al. Absence seizure provocation during routine EEG: Does position of the child during hyperventilation affect the diagnostic yield? Seizure. 2020;79:86–89. doi:10.1016/j.seizure.2020.03.013.
11.
Hourani R, Nasreddine W, et al. When Should a Brain MRI Be Performed in Children with New-Onset Seizures? Results of a Large Prospective Trial. AJNR Am J Neuroradiol. 2021;42(9):1695–1701. doi:10.3174/ajnr.A7193.
12.
Kumar A, Chugani HT. The Role of Radionuclide Imaging in Epilepsy, Part 1: Sporadic Temporal and Extratemporal Lobe Epilepsy. J Nucl Med Technol. 2017;45(1):14–21. doi:10.2967/jnumed.112.114397.
13.
von Oertzen TJ. PET and ictal SPECT can be helpful for localizing epileptic foci. Curr Opin Neurol. 2018;31(2):184–191. doi:10.1097/WCO.0000000000000527.
14.
Thurman DJ, Begley CE, et al. The primary prevention of epilepsy: A report of the Prevention Task Force of the International League Against Epilepsy. Epilepsia. 2018;59(5):905–914. doi:10.1111/epi.14068.
15.
Michelson KA, Lyons TW, et al. Utility of Lumbar Puncture in Children Presenting With Status Epilepticus. Pediatr. Emerg. Care. 2017;33:544–547. doi:10.1097/PEC.0000000000001225.
16.
De Vito A, Mankad K, et al. Narrative review of epilepsy: getting the most out of your neuroimaging. Transl Pediatr. 2021;10(4):1078–1099. doi:10.21037/tp-20-261.
17.
Minardi C, Minacapelli R, et al. Epilepsy in Children: From Diagnosis to Treatment with Focus on Emergency. J Clin Med. 2019;8(1):39. doi:10.3390/jcm8010039.
18.
Scheffer IE, Berkovic S, et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512–521. doi:10.1111/epi.13709.
19.
Zuberi SM, Wirrell E, et al. ILAE classification and definition of epilepsy syndromes with onset in neonates and infants: Position statement by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022;63(6):1349–1397. doi:10.1111/epi.17239.
20.
Specchio N, Wirrell EC, et al. International League Against Epilepsy classification and definition of epilepsy syndromes with onset in childhood: Position paper by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022;63(6):1398–1442. doi:10.1111/epi.17241.
21.
Kaushik JS, Farmania R. Electroencephalography in Paediatric Epilepsy. Indian Pediatr. 2018;55(10):893–901.
22.
Fernandez-Baca Vaca G, Park JT. Focal EEG abnormalities and focal ictal semiology in generalized epilepsy. Seizure. 2020;77:7–14. doi:10.1016/j.seizure.2019.12.013.
23.
Wilmshurst JM, Gaillard WD, et al. Summary of recommendations for the management of infantile seizures: Task Force Report for the ILAE Commission of Paediatric s. Epilepsia. 2015;56(8):1185–97. doi:10.1111/epi.13057.
24.
Thodeson DM, Park JY. Genomic testing in paediatric epilepsy. Cold Spring Harb Mol Case Stud. 2019;5(4):a004135. doi:10.1101/mcs.a004135.
25.
Ream MA, Patel AD. Obtaining genetic testing in paediatric epilepsy. Epilepsia. 2015;56(10):1505–14. doi:10.1111/epi.13122.
26.
Sharma S, Prasad AN. Inborn Errors of Metabolism and Epilepsy: Current Understanding, Diagnosis, and Treatment Approaches. Int J Mol Sci. 2017;18(7):1384. doi:10.3390/ijms18071384.
27.
National Guideline Centre (UK). Evidence review: Prediction of second seizure: Epilepsies in children, young people and adults: diagnosis and management: Evidence review 1. London: National Institute for Health and Care Excellence (NICE); 2022 Apr.
28.
Kumar A, Chugani HT. The Role of Radionuclide Imaging in Epilepsy, Part 2: Epilepsy Syndromes. J Nucl Med Technol. 2017;45(1):22–29. doi:10.2967/jnumed.113.129593.
29.
Papadelis C, Chen YH. Paediatric Magnetoencephalography in Clinical Practice and Research. Neuroimaging Clin N Am. 2020;30(2):239–248. doi:10.1016/j.nic.2020.02.002.
30.
Aung T, Tenney JR, Bagić AI. Contributions of Magnetoencephalography to Understanding Mechanisms of Generalized Epilepsies: Blurring the Boundary Between Focal and Generalized Epilepsies? Front Neurol. 2022;13:831546. doi:10.3389/fneur.2022.831546.
31.
Rzepka-Migut B, Paprocka J. Prospects and Limitations Related to the Use of MicroRNA as a Biomarker of Epilepsy in Children: A Systematic Review. Life (Basel). 2021;11(1):26. doi:10.3390/life11010026.
32.
Ren L, Zhu R, Li X. Silencing miR-181a produces neuroprotection against hippocampus neuron cell apoptosis post-status epilepticus in a rat model and in children with temporal lobe epilepsy. Genet Mol Res. 2016;15 doi:10.4238/gmr.15017798.
33.
Martinez B, Peplow PV. MicroRNAs as potential biomarkers in temporal lobe epilepsy and mesial temporal lobe epilepsy. Neural Regen Res. 2023;18(4):716–726. doi:10.4103/1673-5374.354510.
34.
Gliwińska A, Czubilińska-Łada J, et al. The Role of Brain-Derived Neurotrophic Factor (BDNF) in Diagnosis and Treatment of Epilepsy, Depression, Schizophrenia, Anorexia Nervosa and Alzheimer’s Disease as Highly Drug-Resistant Diseases: A Narrative Review. Brain Sci. 2023;13(2):163. doi:10.3390/brainsci13020163.
35.
Perucca P, Scheffer IE, Kiley M. The management of epilepsy in children and adults. Med J Aust. 2018;208(5):226–233. doi: 0.5694/mja17.00951.
36.
Hakami T. Neuropharmacology of Antiseizure Drugs. Neuropsychopharmacol Rep. 2021;41(3):336–351. doi:10.1002/npr2.12196.
37.
Roger JP, Michael AR. Antiseizure drugs. In: BG Katzung, editor. Basic & clinical pharmacology. McGraw-Hill; 2018. p. 409–39.
38.
Gören MZ, Onat F. Ethosuximide: from bench to bedside. CNS Drug Rev. 2007 Summer;13(2):224–39. doi:10.1111/j.1527-3458.2007.00009.x.
39.
Millership JS, Mifsud J, et al. The metabolism of ethosuximide. Eur J Drug Metab Pharmacokinet. 1993 Oct-Dec;18(4):349–53. doi:10.1007/BF03190184.
40.
Kanner AM, Ashman E, et al. Practice guideline update summary: Efficacy and tolerability of the new antiepileptic drugs II: Treatment-resistant epilepsy: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2018;91(2):82–90. doi:10.1212/WNL.0000000000005756.
41.
Nevitt SJ, Sudell M, et al. Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data. Cochrane Database Syst Rev. 2017;12(12):CD011412. doi:10.1002/14651858.CD011412.pub3.
42.
Beydoun A, DuPont S, et al. Current role of carbamazepine and oxcarbazepine in the management of epilepsy. Seizure. 2020;83:251–263. doi:10.1016/j.seizure.2020.10.018.
43.
Baftiu A, Johannessen Landmark C, et al. Availability of antiepileptic drugs across Europe. Epilepsia. 2015;56(12):e191–7. doi:10.1111/epi.13210.
44.
Das S, Fleming DH, et al. Determination of serum carbamazepine concentration using dried blood spot specimens for resource-limited settings. Hosp Pract (1995). 2017;45(2):46–50. doi:.
45.
Guerreiro CA. Epilepsy: Is there hope? Indian J Med Res. 2016;144(5):657–660. doi:10.4103/ijmr.IJMR_1051_16.
46.
Nair DR. Management of Drug-Resistant Epilepsy. Continuum (Minneap Minn). 2016;22(1 Epilepsy):157–72. doi:10.1212/CON.0000000000000297.
47.
Manford M. Recent advances in epilepsy. J Neurol. 2017;264(8):1811–1824. doi:10.1007/s00415-017-8394-2.
48.
Marson A, Burnside G, et al. SANAD II collaborators. The SANAD II study of the effectiveness and cost-effectiveness of valproate versus levetiracetam for newly diagnosed generalised and unclassifiable epilepsy: an open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet. 2021;397(10282):1375–1386. doi:10.1016/S0140-6736(21)00246-4.
49.
Howard P, Remi J, et al. J Pain Symptom Manage. 2018 Oct;56(4):645–649. doi:10.1016/j.jpainsymman.2018.07.012.
50.
Fang T, Valdes E, et al. Levetiracetam for Seizure Prophylaxis in Neurocritical Care: A Systematic Review and Meta-analysis. Neurocrit Care. 2022 Feb;36(1):248–258. doi:10.1007/s12028-021-01296-z.
51.
Kaur N, Nowacki AS, et al. Cognitive outcomes following paediatric epilepsy surgery. Epilepsy Res. 2022;180:106859. doi:10.1016/j.eplepsyres.2022.106859.
52.
Elliott CA, Broad A, et al. Seizure outcome in paediatric medically refractory temporal lobe epilepsy surgery: selective amygdalohippocampectomy versus anterior temporal lobectomy. J Neurosurg Pediatr. 2018;22(3):276–282. doi:10.3171/2018.4.PEDS17607.
53.
Engel J Jr. The current place of epilepsy surgery. Curr Opin Neurol. 2018;31(2):192–197. doi:10.1097/WCO.0000000000000528.
54.
Joris V, Weil AG, Fallah A. Brain Surgery for Medically Intractable Epilepsy. Adv Pediatr. 2022;69(1):59–74. doi:10.1016/j.yapd.2022.03.014.
55.
Shah AK, Mittal S. Invasive electroencephalography monitoring: Indications and presurgical planning. Ann Indian Acad Neurol. 2014;17(Suppl 1):S89–94. doi:10.4103/0972-2327.128668.
56.
Yang M, Ma Y, et al. A Retrospective Analysis of Stereoelectroencephalography and Subdural Electroencephalography for Preoperative Evaluation of Intractable Epilepsy. Stereotact Funct Neurosurg. 2017;95(1):13–20. doi:10.1159/000453275.
57.
Cossu M, Cardinale F, et al. Stereo-EEG-guided radiofrequency thermocoagulations. Epilepsia. 2017;58 Suppl 1:66–72. doi:10.1111/epi.13687.
58.
Belohlavkova A, Jahodova A, et al. May intraoperative detection of stereotactically inserted intracerebral electrodes increase precision of resective epilepsy surgery? Eur J Paediatr Neurol. 2021;35:49–55. doi:10.1016/j.ejpn.2021.09.012.
59.
Moles A, Guénot M, et al. SEEG-guided radiofrequency coagulation (SEEG-guided RF-TC) versus anterior temporal lobectomy (ATL) in temporal lobe epilepsy. J Neurol. 2018;265(9):1998–2004. doi:10.1007/s00415-018-8958-9.
60.
Chipaux M, Taussig D, et al. SEEG-guided radiofrequency thermocoagulation of epileptic foci in the paediatric population: Feasibility, safety and efficacy. Seizure. 2019;70:63–70. doi:10.1016/j.seizure.2019.07.004.
61.
Hoppe C, Helmstaedter C. Laser interstitial thermotherapy (LiTT) in paediatric epilepsy surgery. Seizure. 2020;77:69–75. doi:10.1016/j.seizure.2018.12.010.
62.
North RY, Raskin JS, Curry DJ. MRI-Guided Laser Interstitial Thermal Therapy for Epilepsy. Neurosurg Clin N Am. 2017;28(4):545–557. doi:10.1016/j.nec.2017.06.001.
63.
Hale AT, Sen S, et al. Open Resection versus Laser Interstitial Thermal Therapy for the Treatment of Paediatric Insular Epilepsy. Neurosurgery. 2019;85(4):E730–E736. doi:10.1093/neuros/nyz094.
64.
Alexander H, Cobourn K, et al. Magnetic resonance-guided laser interstitial thermal therapy for the treatment of non-lesional insular epilepsy in paediatric patients: thermal dynamic and volumetric factors influencing seizure outcomes. Childs Nerv Syst. 2019;35(3):453–461. doi:10.1007/s00381-019-04051-0.
65.
Abdelmoity AT, Le Pichon JB, et al. Combined use of the ketogenic diet and vagus nerve stimulation in paediatric drug-resistant epilepsy. Epilepsia Open. 2021;6(1):112–119. doi:10.1002/epi4.12453.
66.
Aum DJ, Reynolds RA, et al. Surgical outcomes of open and laser interstitial thermal therapy approaches for corpus callosotomy in paediatric epilepsy. Epilepsia. 2023;64(9):2274–2285. doi:10.1111/epi.17679.
67.
Yokosako S, Muraoka N, et al. Corpus callosotomy in paediatric patients with non-lesional epileptic encephalopathy with electrical status epilepticus during sleep. Epilepsy Behav Rep. 2021;16:100463. doi:10.1016/j.ebr.2021.100463.
68.
Baumgartner JE, Blount JP, et al. Technical descriptions of four hemispherectomy approaches: From the Paediatric Epilepsy Surgery Meeting at Gothenburg 2014. Epilepsia. 2017;58 Suppl 1:46–55. doi:10.1111/epi.13679.
69.
Harford E, Houtrow A, et al. Functional outcomes of paediatric hemispherotomy: Impairment, activity, and medical service utilization. Epilepsy Behav. 2023;140:109099. doi:10.1016/j.yebeh.2023.109099.
70.
Griessenauer CJ, Salam S, et al. Hemispherectomy for treatment of refractory epilepsy in the paediatric age group: a systematic review. J Neurosurg Pediatr. 2015;15(1):34–44. doi:10.3171/2014.10.PEDS14155.
71.
Tsai JD, Fan PC, et al. Vagus nerve stimulation in paediatric patients with failed epilepsy surgery. Acta Neurol Belg. 2021;121(5):1305–1309. doi:10.1007/s13760-020-01303-8.
72.
Abdelmoity AT, Le Pichon JB, et al. Combined use of the ketogenic diet and vagus nerve stimulation in paediatric drug-resistant epilepsy. Epilepsia Open. 2021;6(1):112–120. doi:10.1002/epi4.12453.
73.
Wheless JW, Gienapp AJ, Ryvlin P. Vagus nerve stimulation (VNS) therapy update. Epilepsy Behav. 2018;88S:2–10. doi:10.1016/j.yebeh.2018.06.032.
74.
LoPresti MA, Huang J, et al. Vagus nerve stimulator revision in paediatric epilepsy patients: a technical note and case series. Childs Nerv Syst. 2023;39(2):435–441. doi:10.1007/s00381-022-05769-0.
75.
Lotan G, Vaiman M. Treatment of epilepsy by stimulation of the vagus nerve from Head-and-Neck surgical point of view. Laryngoscope. 2015;125(6):1352–5. doi:10.1002/lary.25064.
76.
Piper RJ, Ibrahim GM, Tisdall MM. Deep Brain Stimulation for Children with Generalized Epilepsy. Neurosurg Clin N Am. 2024;35(1):17–25. doi:10.1016/j.nec.2023.09.002.
77.
Wei SH, Lee WT. Comorbidity of childhood epilepsy. J Formos Med Assoc. 2015;114(11):1031–8. doi:10.1016/j.jfma.2015.07.015.
78.
Mula M, Coleman H, Wilson SJ. Neuropsychiatric and Cognitive Comorbidities in Epilepsy. Continuum (Minneap Minn). 2022;28(2):457–482. doi:10.1212/CON.0000000000001123.
79.
Symonds JD, et al. Early childhood epilepsies: epidemiology, classification, aetiology, and socio-economic determinants. Brain. 2021;144(9):2879–2891. doi:10.1093/brain/awab162.
80.
Marcovecchio ML, Petrosino MI, Chiarelli F. Diabetes and epilepsy in children and adolescents. Curr Diab Rep. 2015;15(4):21. doi:10.1007/s11892-015-0588-3.
81.
Perry MS. New and Emerging Medications for Treatment of Paediatric Epilepsy. Pediatr Neurol. 2020;107:24–27. doi:10.1016/j.pediatrneurol.2019.11.008.
82.
Heaney D, Walker MC. Rufinamide. Drugs Today (Barc). 2007;43(7):455–60. doi:10.1358/dot.2007.43.7.1067344.
83.
Eschbach K, Knupp KG. Stiripentol for the treatment of seizures in Dravet syndrome. Expert Rev Clin Pharmacol. 2019;12(5):379–388. doi:10.1080/17512433.2019.1605904.
84.
Tang R, Xu Z. Gene therapy: a double-edged sword with great powers. Mol Cell Biochem. 2020;474(1–2):73–81. doi:10.1007/s11010-020-03834-3.
85.
Zhang L, Wang Y. Gene therapy in epilepsy. Biomed Pharmacother. 2021;143:112075. doi:10.1016/j.biopha.2021.112075.
87.
Turner TJ, et al. Recent advances in gene therapy for neurodevelopmental disorders with epilepsy. J Neurochem. 2021;157(2):229–262. doi:10.1111/jnc.15168.
88.
Billakota S, Devinsky O, Marsh E. Cannabinoid therapy in epilepsy. Curr Opin Neurol. 2019;32(2):220–226. doi:10.1097/WCO.0000000000000660.
89.
Von Wrede R, Helmstaedter C, Surges R. Cannabidiol in the Treatment of Epilepsy. Clin Drug Investig. 2021;41(3):211–220. doi:10.1007/s40261-021-01003-y.
90.
Arzimanoglou A, Brandl U, et al. The Cannabinoids International Experts Panel; Collaborators. Epilepsy and cannabidiol: a guide to treatment. Epileptic Disord. 2020;22(1):1–14. doi:10.1684/epd.2020.1141.
91.
Sampaio LP. Ketogenic diet for epilepsy treatment. Arq Neuropsiquiatr. 2016;74(10):842–848. doi:10.1590/0004-282X20160116.
92.
Ko A, Kwon HE, Kim HD. Updates on the ketogenic diet therapy for paediatric epilepsy. Biomed J. 2022;45(1):19–26. doi:10.1016/j.bj.2021.11.003.
93.
Martin-McGill KJ, Bresnahan R, Levy RG, Cooper PN. Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev. 2020;6(6):CD001903. doi:10.1002/14651858.CD001903.pub5.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.