Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Timing and reasons for lost to follow-up among patients on 6-month standardized anti-TB treatment in Nigeria
1
Jhpiego Nigeria (an affiliate of John Hopkins University), Nigeria
2
Bluegate Research Institute, Ibadan, Nigeria
3
State Ministry of Health, Lagos, Nigeria
Corresponding author
Abiola Victor Adepoju
Jhpiego Nigeria (an affiliate of John Hopkins University), Federal Capital Territory, Wuye, Abuja, Nigeria
Jhpiego Nigeria (an affiliate of John Hopkins University), Federal Capital Territory, Wuye, Abuja, Nigeria
J Pre Clin Clin Res. 2022;16(2):34-37
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Loss to follow-up (LTFU) along the TB care cascade is a barrier to TB control because of sustained TB transmission including resistant strains, high mortality and increased spread of DRTB strains. Understanding common reasons for LTFU and their timing could help target interventions to improve adherence to TB treatment.
Material and methods:
A cross-sectional study using pre-tested questionnaires were administered by phone interviews to 90 TB patients receiving treatment between January – December 2020 who were LTFU while on TB treatment in 31 health facilities across three States in South West Nigeria. The focus of the interviews was to determine the reasons why they were LTFU. Interviewers contacted treatment supporters when patients could not be reached. Clinical and socio-demographic information, such as age, sex and HIV status were extracted from treatment registers
Results:
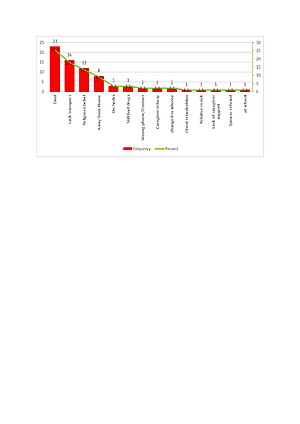
The mean age of patients was 42.6 years (16–90) and SD=17.2. The majority 73 (81%) of LTFU were male, while Ogun State had the highest number – 35 (38.9%), LTFU was highest during the first month on treatment – 60 (66.7%), among HIV negative – 63 (70%), and those who had not been treated previously for TB – 85 (94.4%). The most common reason for LTFU among TB patients on treatment was death – 23(25.6%), followed by lack of transport – 16 (17.8%), and religious beliefs – 12 (13.3%).
Conclusions:
The study suggests a high mortality among patients receiving treatment who may have been classified as LTFU. Interventions to reduce mortality and increase coverage of TB treatment facilities, thus bringing care closer to patients, is necessary. It is suggested that 30-day adherence calendars should be used to improve adherence counselling in the first one month on treatment to minimize early LTFU among TB patients.
Loss to follow-up (LTFU) along the TB care cascade is a barrier to TB control because of sustained TB transmission including resistant strains, high mortality and increased spread of DRTB strains. Understanding common reasons for LTFU and their timing could help target interventions to improve adherence to TB treatment.
Material and methods:
A cross-sectional study using pre-tested questionnaires were administered by phone interviews to 90 TB patients receiving treatment between January – December 2020 who were LTFU while on TB treatment in 31 health facilities across three States in South West Nigeria. The focus of the interviews was to determine the reasons why they were LTFU. Interviewers contacted treatment supporters when patients could not be reached. Clinical and socio-demographic information, such as age, sex and HIV status were extracted from treatment registers
Results:
The mean age of patients was 42.6 years (16–90) and SD=17.2. The majority 73 (81%) of LTFU were male, while Ogun State had the highest number – 35 (38.9%), LTFU was highest during the first month on treatment – 60 (66.7%), among HIV negative – 63 (70%), and those who had not been treated previously for TB – 85 (94.4%). The most common reason for LTFU among TB patients on treatment was death – 23(25.6%), followed by lack of transport – 16 (17.8%), and religious beliefs – 12 (13.3%).
Conclusions:
The study suggests a high mortality among patients receiving treatment who may have been classified as LTFU. Interventions to reduce mortality and increase coverage of TB treatment facilities, thus bringing care closer to patients, is necessary. It is suggested that 30-day adherence calendars should be used to improve adherence counselling in the first one month on treatment to minimize early LTFU among TB patients.
Abiola Victor Adepoju, Ademola Adelekan, Olusola Adedeji Adejumo. Timing and Reasons for Lost to Follow-up among patients on 6-month
standardized anti-TB treatment in Nigeria. J Pre-Clin Clin Res. 2022; 16(2): 34–37. doi: 10.26444/jpccr/150601
REFERENCES (22)
1.
Federal Ministry of Health. Draft Annual TB Report. www.health.gov.ng/doc/Draft-2019-NTBLCP-Annual-report-22032020.pdf (access:2021.05.01).
2.
World Health Organization. Global Tuberculosis Control. https://apps.who.int/iris/bits... (access:2021.04.20).
3.
Xiao H. Drug-Resistant TB. In: Lu Y, Wang L, Duanmu H, editors. Handbook of Global Tuberculosis Control.Ed.2. Boston; 2016. p. 60–64.
4.
Federal Ministry of Health. National tuberculosis and leprosy control programme: workers manual. 5th ed. Abuja; 2008.
5.
Geremew MA, Mulualem T, Gemeda A. Survival Analysis of Loss to Follow-Up Treatment among Tuberculosis Patients at Jimma University Specialized Hospital, Jimma, Southwest Ethiopia. Journal of Stat Mech. 2015;1(1):1–7. https://doi.org/10.1155/2015/9....
6.
World Health Organization. Global Tuberculosis Report. https://apps.who.int/iris/hand... (access:2021.05.01).
7.
Babiarz KS, Suen S, Goldhaber-Fiebert JD. Tuberculosis treatment discontinuation and symptom persistence: an observational study of Bihar, India’s public care system covering >100,000,000 inhabitants. BMC Public Health. 2014;14(1):418. https://doi.org/10.1186/1471-2....
8.
Ruru Y, Matasik M, Oktavian A. Factors associated with non-adherence during tuberculosis treatment among patients treated with DOTS strategy in Jayapura, Papua Province, Indonesia. Global Health Action. 2018;11(1):1–4. https://doi.org/ 10.1080/16549716.2018.1510592.
9.
Roy N, Basu M, Das S. Risk factors associated with default among tuberculosis patients in Darjeeling district of West Bengal. India. J Fam Med Prim Care. 2015;4(1):388–394. https://doi.org/ 10.4103/2249-4863.161330.
10.
Herrero MB, Ramos S, Arrossi S. Determinants of non-adherence to tuberculosis treatment in Argentina: barriers related to access to treatment. Rev. bras. epidemiol. 2015; 18(2): 287–298. https://doi.org/ 10.1590/1980-5497201500020001.
11.
Aung YK, Swe PP, Kyaw Z. Differential loss to follow-up rates among adult tuberculosis patients – Findings from the largest private sector tuberculosis clinic database in Myanmar. PLoS ONE.2019;14(6):1–9. https://doi.org/10.1371/journa....
13.
Macrotrends. Lagos, Nigeria Metro Area Population 1950–2022. https://www.macrotrends.net/ci... (access 2022.05.01).
14.
Zhou TJ, Lakshminarayanan S, Sarkar S. Predictors of Loss to Follow-Up among Men with Tuberculosis in Puducherry and Tamil Nadu, India. The American Journal of Tropical Medicine and Hygeine. 2020;103(3):1050–1056. https://doi.org/10.4269/ajtmh.....
15.
Shaweno T, Getnet M, Fikru C. Does time to loss to follow-up differ among adult tuberculosis patients initiated on tuberculosis treatment and care between general hospital and health centers? A retrospective cohort study. Tropical Medicine and Health. 2020;48(1):9. https://doi.org/10.1186/s41182....
16.
Field N, Lim MS, Murray J. Timing, rates, and causes of death in a large South African tuberculosis programme. BMC Infect Dis. 2014;14(1):1–12. https://doi.org/10.1186/s12879....
17.
Adamu AL, Gadanya MA, Abubakar IS. High mortality among tuberculosis patients on treatment in Nigeria: a retrospective cohort study. BMC Infect Dis. 2017;17(1):170. https://doi.org/10.1186/s12879....
18.
Bisson GP, Zetola N, Collman RG. Persistent high mortality in advanced HIV/TB despite appropriate antiretroviral and antitubercular therapy: an emerging challenge. Current HIV/AIDS Reports. 2015;12(1):107–116. https://doi.org/10.1007/s11904....
19.
1Umo I, Kulai M, Commons RJ. Factors associated with loss to follow-up among TB patients in rural Papua New Guinea. Public Health Action. 2021;21;11(4):186–190.https://doi.org/ 10.5588/pha.21.0054.
20.
Moses I, Main S, Commons RJ. A retrospective study of tuberculosis outcomes in Gulf Province, Papua New Guinea. Public Health Action. 2019;9(1):38–42.https://doi.org/ 10.5588/pha.18.0069.
21.
Sodeng K, Botu A, Semmie M. Challenges in TB diagnosis and treatment: the Kavieng Provincial Hospital experience, Papua New Guinea. Public Health Action. 2019;9(1):57–61. https://doi.org/10.5588/pha.18....
22.
Tupasi TE, Garfin AM, Kurbatova EV. Factors Associated with Loss to Follow-up during Treatment for Multidrug-Resistant Tuberculosis, the Philippines, 2012–2014. Emerg Infect Dis. 2016;22(3):491–502. https://doi.org/10.3201/eid220....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.