Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Symptoms of selected parasitic diseases in the oral cavity
1
Student Research Group, Department of Oral Medicine. Medical University of Lublin, Poland
2
Department of Oral Medicine, Medical University of Lublin, Poland
Corresponding author
Klaudia Lewandowska
Student Research Group, Department of Oral Medicine, Medical University of Lublin, Poland
Student Research Group, Department of Oral Medicine, Medical University of Lublin, Poland
J Pre Clin Clin Res. 2021;15(1):34-39
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Parasitic diseases are caused by many species of protozoa, helminths, and arthropods. Parasitosis can be divided into gastrointestinal, tissue and skin diseases and can appear in many different parts of the body. The most common route of transmission is via ingestion. The oral cavity may be a place of colonization for pathogens, resulting in lesion formation.
Objective:
The aim of the study is to characterise and describe the most important symptoms of parasitic diseases that can be diagnosed during dental examination.
Abbreviated description of the state of knowledge:
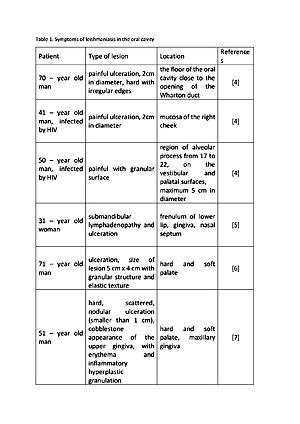
In this study there are discussed diseases caused by the most common protozoa and the nematodes in the oral cavity. Leishmaniasis is caused by Leishmania spp. protozoa, and its most common symptom observed in the oral cavity are painful ulcerations. Toxoplasmosis usually manifests itself through enlargement of the lymph nodes, and the appearance of antibodies in saliva. Entamoeba gingivalis and Trichomonas tenaxcause periodontitis chronica and inflammation of the soft tissue. The first of the nematodes, Gongylonema pulchrum, is the reason for, among others, the itchy sensation of a moving foreign body under the mucosa. The most common symptoms of Ancylostoma infection are erythematous papules. Filariae causes an infection that manifests through swelling, abscesses, and painless nodules inside the mouth.
Conclusions:
New pathogens are emerging worldwide and pose a threat to health. They can manifest their symptoms in the oral cavity, but the diagnosis of the disease by the dentist is not easy and requires interdisciplinary knowledge and consultation.
Parasitic diseases are caused by many species of protozoa, helminths, and arthropods. Parasitosis can be divided into gastrointestinal, tissue and skin diseases and can appear in many different parts of the body. The most common route of transmission is via ingestion. The oral cavity may be a place of colonization for pathogens, resulting in lesion formation.
Objective:
The aim of the study is to characterise and describe the most important symptoms of parasitic diseases that can be diagnosed during dental examination.
Abbreviated description of the state of knowledge:
In this study there are discussed diseases caused by the most common protozoa and the nematodes in the oral cavity. Leishmaniasis is caused by Leishmania spp. protozoa, and its most common symptom observed in the oral cavity are painful ulcerations. Toxoplasmosis usually manifests itself through enlargement of the lymph nodes, and the appearance of antibodies in saliva. Entamoeba gingivalis and Trichomonas tenaxcause periodontitis chronica and inflammation of the soft tissue. The first of the nematodes, Gongylonema pulchrum, is the reason for, among others, the itchy sensation of a moving foreign body under the mucosa. The most common symptoms of Ancylostoma infection are erythematous papules. Filariae causes an infection that manifests through swelling, abscesses, and painless nodules inside the mouth.
Conclusions:
New pathogens are emerging worldwide and pose a threat to health. They can manifest their symptoms in the oral cavity, but the diagnosis of the disease by the dentist is not easy and requires interdisciplinary knowledge and consultation.
Puzio N, Sikora M, Srebrna A, Strączek A, Węglarz N, Lewandowska K, Mazurek G, Thum-Tyzo K. Symptoms of selected parasitic diseases in
the oral cavity. J Pre-Clin Clin Res. 2021; 15(1): 34–39. doi: 10.26444/jpccr/131740
REFERENCES (35)
1.
Hadaś E, Derda M. Pasożyty – zagrożenie nadal aktualne. Probl Hig Epidemiol. 2015; 96(2): 340–343.
2.
Derda M, Hadaś E, Skrzypczak Ł. Pasożyty jamy ustnej. Probl Hig Epidemiol. 2014; 95(1): 6–13.
3.
Gillespie PM, Beaumier CM, Strych U, et al. Status of vaccine research and development of vaccines for leishmaniasis. Vaccine. 2016; 34(26): 2992–2995. https://doi.org/10.1016/j.vacc....
4.
García de Marcos JA, Dean Ferrer A, Alamillos Granados F, et al. Localized Leishmaniasis of the oral mucosa. A report of three cases. Med Oral Patol Oral Cir Bucal. 2007; 12(4): 281–286.
5.
Falcão GGVSC, Lins-Kusterer L, Leite-Ribeiro PM, et al. Orofacial manifestations of mucocutaneous leishmaniasis: a case series from Brazil. F1000Research. 2020; 8: 756. https://doi.org/10.12688/f1000... (access: 2020. 05. 10).
6.
Pellicioli AC, Martins MA, Sant’ana Filho M, et al. Leishmaniasis with oral mucosa involvement. Gerodontology. 2012; 29(2): 1168–1171. ht t ps://doi.org /10.1111/j.1741–2358.2011.0 0512 .x.
7.
Passi D, Sharma S, Dutta S, et al. Localised leishmaniasis of oral mucosa: report of an unusual clinicopathological entity. Case Rep Dent. 2014; 2014: 753149. ht t ps://doi.org /10.1155/2014/753149.
8.
Clem A. A current perspective on leishmaniasis. J Glob Infect Dis. 2010; 2(2): 124–6. https://doi.org/10.4103/0974-7....
9.
Asano S. Granulomatous lymphadenitis. J Clin Exp Hematop. 2012; 52(1): 1–16. https://doi.org /10.3960/jslr t.52.1.
10.
Saxena S, Kumar S, Kharbanda J. Toxoplasmosis submandibular lymphadenitis: Report of an unusual case with a brief review. J Oral Maxillofac Pathol. 2018; 22(1): 116–120. https://doi.org/10.4103/jomfp.... FP_ 2 6 8 _17.
11.
Loyola AM, Durighetto Jr AF, Silva DA, et al. Anti-Toxoplasma gondii immunoglobulins A and G in human saliva and serum. Journal of Oral Pathology&Medicine. 1997; 26(4): 187–91. https://doi.org /10.1111/j.160 0 - 0714.1997.tb0 0456.x.
12.
García G, Ramos F, Martínez-Hernández F, et al. A new subtype of Entamoeba gingivalis: “E. gingivalis ST2, kamaktli variant”. Parasitol Res. 2018; 117(4): 1277–1284. https://doi.org/10.1007/s00436....
13.
Bonner M, Fresno M, Gironès N, et al. Reassessing the Role of Entamoeba gingivalis in Periodontitis. Front Cell Infect Microbiol. 2018; 8: 379. https://doi.org/10.3389/fcimb.....
14.
Garcia G, Ramos F, Maldonado J, et al. Prevalence of two Entamoeba gingivalis ST1 and ST2-kamaktli subtypes in the human oral cavity under various conditions. Parasitol. Res. 2018; 117(9): 2941–2948. https://doi.org/10.1007/s00436....
15.
Bao X, Wiehe R, Dommisch H, et al. Entamoeba gingivalis Causes Oral Inflammation and Tissue Destruction. Journal of Dental Research. 2020; 99(5): 561–567. https://doi.org/10.1177/002203....
16.
Bonner MM, Amard V, Bar-Pinatel C, et al. Detection of the amoeba Entamoeba gingivalis in periodontal pockets. Parasite. 2014; 21: 30. https://doi.org/10.1051/parasi....
17.
Morozińska-Gogol J. Parazytologia medyczna. Kompendium. Warszawa: Wydawnictwo Lekarskie PZWL; 2016. p. 320.
18.
Ribeiro LC, Santos C, Benchimol M. Is Trichomonas tenax a Parasite or a Commensal? Protis. 2015; 166(2): 196–210. https://doi.org/10.1016/j.prot....
19.
Marty M, Lemaitre M, Kémoun P, et al. Trichomonas tenax and periodontal diseases: a concise review. Parasitology. 2017; 144(11): 1417–1425. https://doi.org/10.1017/S00311....
20.
Benabdelkader S, Andreani J, Gillet A, et al. Specific clones of Trichomonas tenax are associated with periodontitis. PLoS One. 2019; 14(3). https://doi.org/10.1371/journa....
21.
Dudko A, Kurnatowska AJ. Występowanie Trichomonas tenax i grzybów u pacjentów z chorobami przyzębia. Mikol Lek. 2007; 14(4): 227–232.
22.
Sarowska J, Wojnicz D, Kaczkowski H, et al. Występowanie entamoeba gingivalis i trichomonas tenax u pacjentów ze schorzeniami przyzębia, w stanie immunosupresji i z chorobami genetycznymi. Adv Clin Exp Med. 2004; 13(2): 291–297.
23.
Derda M, Hadaś E, Antczak E, et al. Częstość występowania Entamoeba gingivalis w jamie ustnej studentów. J Stoma. 2011; 64(10): 784–795.
24.
Wantland WW, Lauer D. Correlation of some oral hygiene variables with age, sex, and incidence of oral Protozoa. J Dent Res. 1970; 49(2): 293–297. https://doi.org/10.1177%2F0022....
25.
Hassona Y, Scully C, Delgado-Azanero W, et al. Oral helminthic infestations. Journal of investigative and clinical dentistry. 2015; 6(2): 99–107. https://doi.org/10.1111/jicd.1....
26.
Rachmawati E, Murniati N, Yohana W. Oral Manifestation of Helminth Infection Due to Nematode. Journal of Advanced Medical and Dental Sciences Research. 2019; 7(8): 211–213. https://doi.org/10.21276/jamds....
27.
Kramar U, Skvarč M, Logar M, et al. First case of human Gongylonema pulchrum infection in Slovenia. J Helminthol. 2019; 22(94): 62. https://doi.org/10.1017/S00221....
28.
Xiaodan L, Zhensheng W, Ying H, et al. Gongylonema pulchrum infection in the human oral cavity: A case report and literature review. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 2018; 125(3): 49–53. https://doi.org/10.1016/j.oooo....
29.
Huang Q, Wang J, Yang T, et al. Multiple Gongylonema pulchrum worms in a human esophagus. Endoscopy. 2016; 48: 24–25. https://doi.org/10.1055/s-0035....
30.
Pesson B, Hersant C, Biehler JF, et al. First Case of Human Gongylo-nemosis in France. Parasite. 2013; 20: 5. https://doi.org/10.1051/parasi....
31.
Allen JD, Esquela-Kerscher A. Short report: Gongylonema pulchrum infection in a resident of williamsburg, Virginia, verified by genetic analysis. Am J Trop Med Hyg. 2013; 89(4): 755–757. https://doi.org/10.4269/ajtmh.....
32.
Libertin CR, Reza M, Peterson JH, et al. Case report: Human gongylonema pulchrum infection: Esophageal symptoms and need for prolonged albendazole therapy. Am J Trop Med Hyg. 2017; 96(4): 873–875. https://doi.org/10.4269/ajtmh.....
33.
Xiao-Li Y. One case of Gongylonema pulchrum infection in esophagus in human. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. 2016; 29(1): 126 –128. https://doi.org/10.1016/j.oooo....
34.
Damante JH, Chinellato LEM, de Oliveira FT, et al. Larva migrans in the oral mucosa: Report of two cases. Braz. Dent. J. 2011; 22(2): 166–170. https://doi.org/10.1590/S0103-....
35.
Lupi O, Downing C, Lee M, et al. Mucocutaneous manifestations of helminth infections: Nematodes. Journal of the American Academy of Dermatology. 2015; 73(6): 929–944. https://doi.org/10.1016/j.jaad....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.