Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Post-herpetic neuralgia: currently available oral and topical medications in the management of pain – a review
1
Clinical Department of Internal Medicine, 4th Military Clinical Hospital, Wrocław, Poland
2
Clinical Department of Endocrinology, Metabolic and Internal Medicine, University Clinical Hospital, Poznań Poland
3
Internal Medicine Department, Rear Admiral Professor Wiesław Łasiński 7th Military Navy Hospital, Gdańsk, Poland
4
SPZOZ of the Ministry of Internal Affairs and Administration, Department of Internal Medicine and Geriatrics, Krakow, Poland
5
Department of Clinical Oncology, PCK Maritime Hospital, Gdynia, Poland
6
Department of Gastroenterology and Internal Medicine, Autonomous Public Provincial Polyclinical Hospital, Szczecin, Poland
Corresponding author
Damian Bęben
4th Military Clinical Hospital, Clinical Department of Internal Medicine, Weigla 5 Street, 53-114, Wrocław, Poland
4th Military Clinical Hospital, Clinical Department of Internal Medicine, Weigla 5 Street, 53-114, Wrocław, Poland
J Pre Clin Clin Res. 2024;18(2):162-167
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Post-herpetic neuralgia (PHN) is the most common chronic complication of herpes zoster and also one of the most troublesome. It is a prime example of typical neuropathic pain which in many cases contributes to a significant reduction in the patient’s quality of life. Despite the emergence of a prophylactic method in the form of a vaccine, PHN continues to be a significant problem, particularly affecting the elderly and immunocompromised individuals.
Objective:
The aim of this review is to summarize the knowledge contained in the current literature on the available oral and topical medications for the treatment of neuropathic pain in PHN. An area of particular focus was the effectiveness and safety of their use
Review methods:
The review is based on 49 scientific publications found in PubMed, PubMedCentral, NCBI and Via Medica Journals databases published between 2008–2024.
Brief description of the state of knowledge:
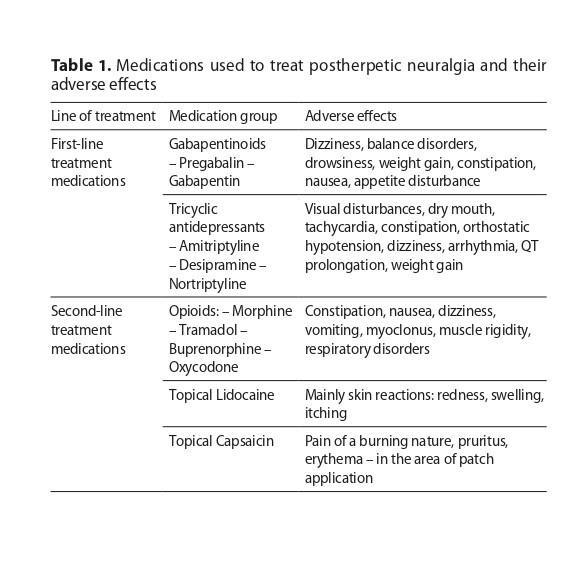
Current treatment of PHN is mainly based on pharmacological therapy. Both oral and topical drugs belonging to a variety of groups are used. Gabapentinoids, tricyclic anti-depressants and, in some circumstances, lidocaine 5% patches, are considered first-line medications. In contrast, capsaicin 8% and opioids are considered second-line medications. The use of multimodal therapy is becoming widespread due to the relatively frequent ineffectiveness of pain management during monotherapy.
Summary:
Despite the wide range of methods available for use in the treatment of neuropathic pain, management of PHN continues to be a challenging task. Multimodal therapy using medications with different mechanisms of action and an individualized approach to drug selection based on the specific clinical case are crucial for treatment success.
Post-herpetic neuralgia (PHN) is the most common chronic complication of herpes zoster and also one of the most troublesome. It is a prime example of typical neuropathic pain which in many cases contributes to a significant reduction in the patient’s quality of life. Despite the emergence of a prophylactic method in the form of a vaccine, PHN continues to be a significant problem, particularly affecting the elderly and immunocompromised individuals.
Objective:
The aim of this review is to summarize the knowledge contained in the current literature on the available oral and topical medications for the treatment of neuropathic pain in PHN. An area of particular focus was the effectiveness and safety of their use
Review methods:
The review is based on 49 scientific publications found in PubMed, PubMedCentral, NCBI and Via Medica Journals databases published between 2008–2024.
Brief description of the state of knowledge:
Current treatment of PHN is mainly based on pharmacological therapy. Both oral and topical drugs belonging to a variety of groups are used. Gabapentinoids, tricyclic anti-depressants and, in some circumstances, lidocaine 5% patches, are considered first-line medications. In contrast, capsaicin 8% and opioids are considered second-line medications. The use of multimodal therapy is becoming widespread due to the relatively frequent ineffectiveness of pain management during monotherapy.
Summary:
Despite the wide range of methods available for use in the treatment of neuropathic pain, management of PHN continues to be a challenging task. Multimodal therapy using medications with different mechanisms of action and an individualized approach to drug selection based on the specific clinical case are crucial for treatment success.
Bęben D, Kowalewski J, Recka K, Michałka D, Grzelak A, Jędrocha O, Godyńska S, Obacz E, Grodek Z, Miliwek J. Postherpetic neuralgia:
Currently available oral and topical medications in the management of pain – a review. J Pre-Clin Clin Res. 2024; 18(2): 162–167. doi: 10.26444/jpccr/189442
REFERENCES (49)
1.
Johnson RW, Rice AS. Clinical practice. Postherpetic neuralgia. N Engl J Med. 2014;371(16):1526–1533. doi:10.1056/NEJMcp1403062.
2.
Gruver C, Guthmiller KB. Postherpetic Neuralgia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; April 17, 2023.
3.
Philip A, Thakur R. Post herpetic neuralgia. J Palliat Med. 2011;14(6):765–773. doi:10.1089/jpm.2011.9685.
4.
Schutzer-Weissmann J, Farquhar-Smith P. Post-herpetic neuralgia – a review of current management and future directions. Expert Opin Pharmacother. 2017;18(16):1739–1750. doi:10.1080/14656566.2017.1392508.
5.
Nair PA, Patel BC. Herpes Zoster. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 4, 2023.
6.
Niemeyer CS, Harlander-Locke M, Bubak AN, et al. Trigeminal Postherpetic Neuralgia: From Pathophysiology to Treatment. Curr Pain Headache Rep. 2024;28(4):295–306. doi:10.1007/s11916-023-01209-z.
7.
Feller L, Khammissa RAG, Fourie J, et al. Postherpetic Neuralgia and Trigeminal Neuralgia. Pain Res Treat. 2017;2017:1681765. doi:10.1155/2017/1681765.
8.
Mallick-Searle T, Snodgrass B, Brant JM. Postherpetic neuralgia: epidemiology, pathophysiology, and pain management pharmacology. J Multidiscip Healthc. 2016;9:447–454. Published 2016 Sep 21. doi:10.2147/JMDH.S106340.
9.
Andres TM, McGrane T, McEvoy MD, et al. Geriatric Pharmacology: An Update. Anesthesiol Clin. 2019;37(3):475–492. doi:10.1016/j.anclin.2019.04.007.
10.
Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):1113-e88. doi:10.1111/j.1468-1331.2010.02999.x.
11.
Gross GE, Eisert L, Doerr HW, et al. S2k guidelines for the diagnosis and treatment of herpes zoster and postherpetic neuralgia. J Dtsch Dermatol Ges. 2020;18(1):55–78. doi:10.1111/ddg.14013.
12.
Liu X, Wei L, Zeng Q, et al. The Treatment of Topical Drugs for Postherpetic Neuralgia: A Network Meta-Analysis. Pain Physician. 2020;23(6):541–551.
13.
Chincholkar M. Gabapentinoids: pharmacokinetics, pharmacodynamics and considerations for clinical practice. Br J Pain. 2020;14(2):104–114. doi:10.1177/2049463720912496.
14.
Athavale A, Murnion B. Gabapentinoids: a therapeutic review. Aust Prescr. 2023;46(4):80–85. doi:10.18773/austprescr.2023.025.
15.
Bockbrader HN, Wesche D, Miller R, et al. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010;49(10):661–669. doi:10.2165/11536200-000000000-00000.
16.
Hadley GR, Gayle JA, Ripoll J, et al. Post-herpetic Neuralgia: a Review [published correction appears in Curr Pain Headache Rep. 2016 Apr;20(4):28]. Curr Pain Headache Rep. 2016;20(3):17. doi:10.1007/s11916-016-0548-x.
17.
Wiffen PJ, Derry S, Bell RF, et al. Gabapentin for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2017;6(6):CD007938. Published 2017 Jun 9. doi:10.1002/14651858.CD007938.pub4.
18.
Sang CN, Sathyanarayana R, Sweeney M; DM-1796 Study Investigators. Gastroretentive gabapentin (G-GR) formulation reduces intensity of pain associated with postherpetic neuralgia (PHN). Clin J Pain. 2013;29(4):281–288. doi:10.1097/AJP.0b013e318258993e.
19.
Swearingen D, Aronoff GM, Ciric S, et al. Pharmacokinetics of immediate release, extended release, and gastric retentive gabapentin formulations in healthy adults. Int J Clin Pharmacol Ther. 2018;56(5):231–238. doi:10.5414/CP203166.
20.
Schulze-Bonhage A. Pharmacokinetic and pharmacodynamic profile of pregabalin and its role in the treatment of epilepsy. Expert Opin Drug Metab Toxicol. 2013;9(1):105–115. doi:10.1517/17425255.2013.749239.
21.
Cao X, Shen Z, Wang X, et al. A Meta-analysis of Randomized Controlled Trials Comparing the Efficacy and Safety of Pregabalin and Gabapentin in the Treatment of Postherpetic Neuralgia. Pain Ther. 2023;12(1):1–18. doi:10.1007/s40122-022-00451-4.
22.
Mathieson S, Lin CC, Underwood M, et al. Pregabalin and gabapentin for pain. BMJ. 2020;369:m1315. Published 2020 Apr 28. doi:10.1136/bmj.m1315.
23.
Mersfelder TL, Nichols WH. Gabapentin: Abuse, Dependence, and Withdrawal. Ann Pharmacother. 2016;50(3):229–233. doi:10.1177/1060028015620800.
24.
Massengill JS, Kittredge JL. Practical considerations in the pharmacological treatment of postherpetic neuralgia for the primary care provider. J Pain Res. 2014;7:125–132. Published 2014 Mar 10. doi:10.2147/JPR.S57242.
25.
Schneider J, Patterson M, Jimenez XF. Beyond depression: Other uses for tricyclic antidepressants. Cleve Clin J Med. 2019;86(12):807–814. doi:10.3949/ccjm.86a.19005.
26.
Hiroki T, Suto T, Saito S, et al. Repeated Administration of Amitriptyline in Neuropathic Pain: Modulation of the Noradrenergic Descending Inhibitory System. Anesth Analg. 2017;125(4):1281–1288. doi:10.1213/ ANE.0000000000002352.
27.
Shrestha M, Chen A. Modalities in managing postherpetic neuralgia. Korean J Pain. 2018;31(4):235–243. doi:10.3344/kjp.2018.31.4.235.
28.
Birkinshaw H, Friedrich CM, Cole P, et al. Antidepressants for pain management in adults with chronic pain: a network meta-analysis. Cochrane Database Syst Rev. 2023;5(5):CD014682. Published 2023 May 10. doi:10.1002/14651858.CD014682.pub2.
29.
Hearn L, Moore RA, Derry S, et al. Desipramine for neuropathic pain in adults. Cochrane Database Syst Rev. 2014;2014(9):CD011003. Published 2014 Sep 23. doi:10.1002/14651858.CD011003.pub2.
30.
Derry S, Wiffen PJ, Aldington D, et al. Nortriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;1(1):CD011209. Published 2015 Jan 8. doi:10.1002/14651858.CD011209.pub2.
31.
Thour A, Marwaha R. Amitriptyline. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 18, 2023.
32.
Moraczewski J, Awosika AO, Aedma KK. Tricyclic Antidepressants. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 17, 2023.
33.
Przewlocka B. Basic mechanisms of analgesic effects of opioids. Palliat Med Pract. 2017;11(2):48–54.
34.
Smith HS. Opioids and neuropathic pain. Pain Physician. 2012;15(3 Suppl):ES93-ES110.
35.
Tsoleridis T. The Use of Transdermal Buprenorphine for Acute Postherpetic Neuralgia: A Case Report. Cureus. 2023;15(2):e34886. Published 2023 Feb 12. doi:10.7759/cureus.34886.
36.
Huerta MÁ, Garcia MM, García-Parra B, et al. Investigational Drugs for the Treatment of Postherpetic Neuralgia: Systematic Review of Randomized Controlled Trials. Int J Mol Sci. 2023;24(16):12987. Published 2023 Aug 20. doi:10.3390/ijms241612987.
37.
Zaporowska-Stachowiak I, Oduah MT, Celichowska M, et al. Opioids in clinical practice. Palliat Med Pract. 2020;13(4):221–228. doi:10.5603/ pmpi.2019.0024.
38.
Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105–S120.
39.
Wordliczek J, Zajączkowska R, Leppert W. Pharmacotherapy of neuropathic pain. Palliat Med Pract. 2017;11(2):61–73. doi:10.5603/ PMPI.2020.0020.
40.
Casale R, Di Matteo M, Minella CE, et al. Reduction of painful area as new possible therapeutic target in post-herpetic neuropathic pain treated with 5% lidocaine medicated plaster: a case series. J Pain Res. 2014;7:353–357. Published 2014 Jun 23. doi:10.2147/JPR.S65398.
41.
Binder A, Bruxelle J, Rogers P, et al. Topical 5% lidocaine (lignocaine) medicated plaster treatment for post-herpetic neuralgia: results of a double-blind, placebo-controlled, multinational efficacy and safety trial. Clin Drug Investig. 2009;29(6):393–408. doi:10.2165/00044011-200929060-00003.
42.
Voute M, Morel V, Pickering G. Topical Lidocaine for Chronic Pain Treatment. Drug Des Devel Ther. 2021;15:4091–4103. Published 2021 Sep 29. doi:10.2147/DDDT.S328228.
43.
Baron R, Allegri M, Correa-Illanes G, et al. The 5% Lidocaine-Medicated Plaster: Its Inclusion in International Treatment Guidelines for Treating Localized Neuropathic Pain, and Clinical Evidence Supporting its Use. Pain Ther. 2016;5(2):149–169. doi:10.1007/s40122-016-0060-3.
44.
Goncalves D, Rebelo V, Barbosa P, et al. 8% Capsaicin Patch in Treatment of Peripheral Neuropathic Pain. Pain Physician. 2020;23(5):E541–E548.
45.
Santos MP, Lemos F, Gomes J, et al. Topical capsaicin 8% patch in peripheral neuropathic pain: Efficacy and quality of life. Br J Pain. 2024;18(1):42–56. doi:10.1177/20494637231201502.
46.
Boccella S, De Filippis L, Giorgio C, et al. Combination Drug Therapy for the Management of Chronic Neuropathic Pain. Biomolecules. 2023;13(12):1802. Published 2023 Dec 16. doi:10.3390/biom13121802.
47.
Guimarães Pereira JE, Ferreira Gomes Pereira L, Mercante Linhares R, et al. Efficacy and Safety of Ketamine in the Treatment of Neuropathic Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Pain Res. 2022;15:1011–1037. Published 2022 Apr 9. doi:10.2147/JPR.S358070.
48.
Rice ASC, Dworkin RH, Finnerup NB, et al. Efficacy and safety of EMA401 in peripheral neuropathic pain: results of 2 randomised, double-blind, phase 2 studies in patients with postherpetic neuralgia and painful diabetic neuropathy. Pain. 2021;162(10):2578–2589. doi:10.1097/j.pain.0000000000002252.
49.
Keppel Hesselink JM, Schatman ME. EMA401: an old antagonist of the AT2R for a new indication in neuropathic pain. J Pain Res. 2017;10:439–443. Published 2017 Feb 20. doi:10.2147/JPR.S128520.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.