Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Congenital tracheobronchial branching anomalies – types and clinical significance.
1
Human Anatomy Research Group, Medical University, Lublin, Poland
2
1st Military Clinical Hospital with the Outpatient Clinic, Lublin, Poland
3
Department of Correct, Clinical and Imaging Anatomy, Medical University, Lublin, Poland
Corresponding author
J Pre Clin Clin Res. 2024;18(2):151-155
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Objective.The tracheobronchial tree consists of the pathways through which air reaches the pulmonary alveoli. Anomalies in the tracheobronchial tree can be both congenital and acquired. Congenital anomalies include tracheal bronchus, accessory cardiac bronchus, lung aplasia, hypoplasia, or agenesis. The aim of this review is to summarise knowledge about the most common congenital anomalies in the tracheobronchial tree, and associated symptoms.
Review methods:
The review was created based on 19 papers found in PubMed and PubMedCentral databases after searching for: ’tracheobronchial branches abnormality’, ‘tracheal bronchus’, and ‘accessory cardiac bronchus’, published between 2001–2023.
Brief description of the state of knowledge:
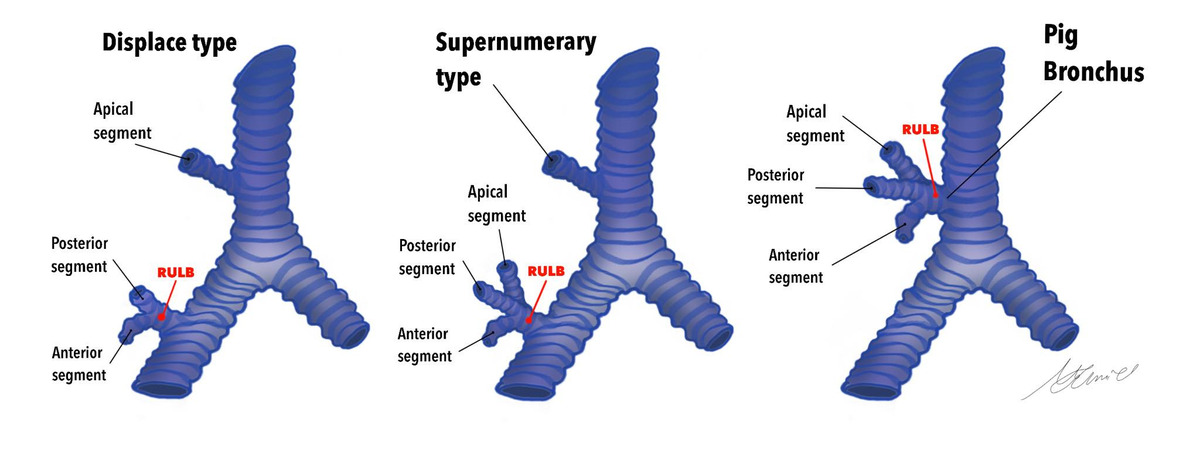
Accessory cardiac bronchus (ACB) and tracheal bronchus (TB) are the 2 most common congenital anomalies of the tracheobronchial tree. The incidence of ACB ranges from 0.07% – 0.5%, and TB between 0.9% – 3% There are 3 types of ACB, with type I being the most common. TB is most frequently detected on the right side. Both anomalies are often asymptomatic; however, diagnosing them may be crucial in cases of recurrent symptoms of unknown origin, such as cough, haemoptysis or recurrent pneumonia. They may also contribute to complications in surgical procedures conducted on the respiratory tract or within the chest cavity.
Summary:
Understanding the occurrence of anatomical anomalies in the branching of the tracheobronchial tree can facilitate the diagnosis of atypical respiratory symptoms and clarify the cause of procedural failures, such as bronchoscopy, intubation or thoracic surgery.
Objective.The tracheobronchial tree consists of the pathways through which air reaches the pulmonary alveoli. Anomalies in the tracheobronchial tree can be both congenital and acquired. Congenital anomalies include tracheal bronchus, accessory cardiac bronchus, lung aplasia, hypoplasia, or agenesis. The aim of this review is to summarise knowledge about the most common congenital anomalies in the tracheobronchial tree, and associated symptoms.
Review methods:
The review was created based on 19 papers found in PubMed and PubMedCentral databases after searching for: ’tracheobronchial branches abnormality’, ‘tracheal bronchus’, and ‘accessory cardiac bronchus’, published between 2001–2023.
Brief description of the state of knowledge:
Accessory cardiac bronchus (ACB) and tracheal bronchus (TB) are the 2 most common congenital anomalies of the tracheobronchial tree. The incidence of ACB ranges from 0.07% – 0.5%, and TB between 0.9% – 3% There are 3 types of ACB, with type I being the most common. TB is most frequently detected on the right side. Both anomalies are often asymptomatic; however, diagnosing them may be crucial in cases of recurrent symptoms of unknown origin, such as cough, haemoptysis or recurrent pneumonia. They may also contribute to complications in surgical procedures conducted on the respiratory tract or within the chest cavity.
Summary:
Understanding the occurrence of anatomical anomalies in the branching of the tracheobronchial tree can facilitate the diagnosis of atypical respiratory symptoms and clarify the cause of procedural failures, such as bronchoscopy, intubation or thoracic surgery.
Syga K, Lewtak J, Iwaniuk K, Stanicki P, Białkowska Z, Daniluk A, Buczek J, Samczuk M, Stachowicz H, Ostański J. Congenital tracheobronchial
branching anomalies – types and clinical significance. J Pre-Clin Clin Res. 2024; 18(2): 151–155. doi: 10.26444/jpccr/187202
REFERENCES (19)
1.
Desir A, Ghaye B. Congenital abnormalities of intrathoracic airways. Radiol Clin North Am. 2009;47(2):203–225. doi:10.1016/J.RCL.2008.11.009.
2.
Ghaye B, Szapiro D, Fanchamps JM, Dondelinger RF. Congenital bronchial abnormalities revisited. Radiographics. 2001;21(1):105–119. doi:10.1148/RADIOGRAPHICS.21.1.G01JA06105.
3.
Wooten C, Patel S, Cassidy L, et al. Variations of the tracheobronchial tree: anatomical and clinical significance. Clin Anat. 2014;27(8):1223–1233. doi:10.1002/CA.22351.
4.
Chaddha U, Chang CF, Lee C. Congenital Tracheobronchial Branching Anomalies. Ann Am Thorac Soc. 2018;15(8):995–997. doi:10.1513/ANNALSATS.201802–088CC.
6.
Chassagnon G, Morel B, Carpentier E, Le Pointe HD, Sirinelli D. Tracheobronchial branching abnormalities: Lobe-based classification scheme. Radiographics. 2016;36(2):358–373. doi:10.1148/rg.2016150115.
7.
Marini T, Hobbs SK, Chaturvedi A, Kaproth-Joslin K. Beyond bronchitis: a review of the congenital and acquired abnormalities of the bronchus. Insights Imaging. 2017;8(1):141–153. doi:10.1007/s13244–016–0537-y.
8.
Acar T, Bayraktaroglu S, Ceylan N, Savas R. Computed tomography findings of tracheobronchial system diseases: a pictorial essay. Jpn J Radiol. 2015;33(2):51–58. doi:10.1007/S11604–014–0380–3.
9.
Sabri YY, Yamamah HGAEN, Taymour TA. Role of multislice computed tomography in evaluation of congenital tracheobronchial branching anomalies. The Egyptian Journal of Radiology and Nuclear Medicine. 2018;49(4):1003–1008. doi:10.1016/J.EJRNM.2018.06.017.
10.
Dogra N, Singla K, Kajal K, Mahajan S, Biswas I. Unusual “cardiac” cause of hemoptysis: Accessory cardiac bronchus. Ann Card Anaesth. 2021;24(3):419. doi:10.4103/ACA.ACA_118_19.
11.
de la Sota-Montero R, García-Lujan R, de Granda-Orive JI. A Rare Cause of Hemoptysis: Accessory Cardiac Bronchus. Arch Bronconeumol. 2023;59(10):668–669. doi:10.1016/J.ARBRES.2023.07.030.
12.
Wong LM, Cheruiyot I, de Oliveira MHS, et al. Congenital Anomalies of the Tracheobronchial Tree: A Meta-Analysis and Clinical Considerations. Ann Thorac Surg. 2021;112(1):315–325. doi:10.1016/J.ATHORACSUR.2020.08.060.
13.
Sun L, Dong L, Jia X, Chen Y, Zhang S, Zhang H. Epidemiological studies of accessory cardiac bronchus and a new variant. Quant Imaging Med Surg. 2022;12(8):4296–4303. doi:10.21037/QIMS-22–68.
14.
Köybaşi G, Satici C, Demir U, Atasever F, Özdemir C, Koşar F. Airflow patterns in the trachebronchial tree of a patient with an accessory cardiac bronchus: A rare congenital anomaly. Tuberk Toraks. 2022;70(3):293–297. doi:10.5578/TT.20229709.
15.
Trisolini R, Paioli D, Betti S, Livi V, Mehta AC. Carinal bronchus: A unique variant of the accessory cardiac bronchus. Am J Respir Crit Care Med. 2020;202(3):E70-E71. doi:10.1164/RCCM.201911–2294IM.
16.
Jamil A, Soos MP. Tracheal Bronchus. StatPearls. Published online June 12, 2023. Accessed November 27, 2023. https://www.ncbi.nlm.nih.gov/b....
17.
Al-Naimi A, Hamad S, Abushahin A. Tracheal Bronchus and Associated Anomaly Prevalence Among Children. Cureus. 2021;13(5). doi:10.7759/CUREUS.15192.
18.
Pérez Ruiz E, Caro Aguilera P, Valdivielso AI, Sanchís Cárdenas S, Martínez García Y, Pérez Frías J. Tracheal bronchus diagnosed in children undergoing flexible bronchoscopy. Paediatr Respir Rev. 2018;28:26–30. doi:10.1016/J.PRRV.2018.03.009.
19.
Panigrahi MK, Pradhan G, Mohapatra PR. Tracheal bronchus presenting with recurrent haemoptysis in an adult female. Adv Respir Med. 2017;85(3):155–157. doi:10.5603/ARM.2017.0026.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.