Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
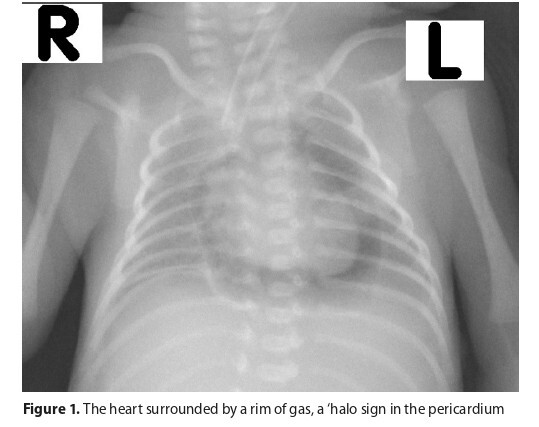
Pneumopericardium in a preterm infant with severe Respiratory Distress Syndrome
1
Students’ Scientific Association at the Department of Paediatric Haematology, Oncology and Transplantation, Medical University, Lublin, Poland
2
Department of Neonatology and Neonatal Intensive Care Unit, Pro-Familia Specialist Hospital,Poland
Corresponding author
Wojciech Stanisław Homa
Students’ Scientific Association at the Department of Pediatric Hematology, Oncology and Transplantation, Medical University of Lublin, ul. prof. Antoniego Gębali 6, 20–093, Lublin, Poland
Students’ Scientific Association at the Department of Pediatric Hematology, Oncology and Transplantation, Medical University of Lublin, ul. prof. Antoniego Gębali 6, 20–093, Lublin, Poland
J Pre Clin Clin Res. 2025;19(2):57-59
KEYWORDS
TOPICS
ABSTRACT
Neonatal pneumopericardium (NPPC) is a rare clinical condition that typically occurs alongside other air leak syndromes. The
key risk factors of its occurrence are advanced lung pathologies treated with high-pressure mechanical ventilation. The most
severe form of NPCC is its tension form, which induces cardiac tamponade and may result in sudden cardiac arrest. Surfactant
replacement therapy is currently the only pharmacological prophylaxis to prevent NPPC. In patients with a stable clinical
condition, high-concentration oxygen therapy is the primary treatment option. If PPC complicates with cardiac tamponade,
immediate pericardiocentesis remains the only effective intervention. A case is presented of a premature infant with severe
respiratory distress syndrome (RDS) who developed an isolated tension form of PPC, complicated with cardiac tamponade
Wanat J, Homa WS, Homa PK, Homa E, Terpin AP, Zawora A. Pneumopericardium in a Preterm Infant with Severe Respiratory Distress Syndrome. J Pre-Clin Clin Res. 2025;19(2):57–59. doi:10.26444/jpccr/204549
REFERENCES (24)
1.
Bonardi CM, Spadini S, Fazio PC, et al. Nontraumatic tension pneumopericardium in nonventilated pediatric patients: a review. J Card Surg. 2019;34(9):829–36. https://doi.org/10.1111/jocs.1....
2.
Beaton A, Sendi P, Martinez PA, et al. Prevalence and outcomes of air leak syndrome and subtypes in neonates in the United States. J Neonatal Perinatal Med. 2024;17(6):846–57. https://doi.org/10.1177/193457....
3.
Sinha SK, Aggarwal P, Samrat S, et al. Isolated pneumopericardium; An extremely rare complication following active resuscitation in a term neonate. ARYA Atheroscler. 2021;17(1): 1–4. https://doi.org/10.22122/arya.....
4.
Garvey A, Filan P. Neonatal pneumopericardium. Arch Dis Child Fetal Neonatal Ed. 2019;104(5):479. https://doi.org/10.1136/archdi....
5.
Tesnière M, Kovacic L, Hedreville N, et al. Tension pneumopericardium in an infant with acute respiratory distress syndrome. Pediatr Neonatol. 2020;61(4):451–52. https://doi.org/10.1016/j.pedn....
6.
Hook B, Hack M, Morrison S, et al. Pneumopericardium in very low birth weight infants. J Perinatol. 1995;15(1):27–31.
7.
Rupprecht H, Gaab K. Tension pneumopericardium in a multiply injured child. Asian Cardiovasc Thorac Ann. 2017;25(7–8):550 52. https://doi.org/10.1177/021849....
8.
Tani M, Kanazawa T, Shioji N, et al. Successful treatment with positive airway pressure ventilation for tension pneumopericardium after pericardiocentesis in a neonate: a case report. JA Clin Rep. 2020;6(1):79. https://doi.org/10.1186/S40981....
9.
Haley A, Mishra PK, Bany-Mohammed F. Spontaneous pneumo-pericardium in a term newborn: a case report. Int J Radiol Radiat Ther. 2018;5(2):129–31. https://doi.org/10.15406/ijrrt....
10.
Roychoudhury S, Kaur S, Soraisham AS. Neonatal Pneumopericardium in a Nonventilated Term Infant: A Case Report and Review of the Literature. Case Rep Pediatr. 2017;2017:3149370. https://doi.org/10.1155/2017/3....
11.
Maxson IN, Chandnani HK, Lion RP. The Heart’s Halo: Caring for Pediatric Pneumopericardium. J Pediatr Intensive Care. 2018;7(4):213–15. https://doi.org/10.1055/S-0038....
12.
Suresh P, Tagare A, Kadam S, et al. Spontaneous pneumopericardium in a healthy full-term neonate. Indian J Pediatr. 2011;78(11):1410–11. https://doi.org/10.1007/s12098....
13.
Satheeshkumar D, Kumaravel KS, Karuna C, et al. A Case of Conservatively Managed Pneumopericardium in a Neonate. Pediatr Oncall J. 2018;15:114. https://doi.org/10.7199/ped.on....
14.
Bhat AP, Pimpalwar A, Dyke II PC. Ultrasonography and X-Ray guided drain placement to evacuate a pneumopericardium/ pneumomediastinum in a 1-day-old infant. Indian J Radiol Imaging. 2019;29(1):94–97. https://doi.org/10.4103/ijri.I....
15.
Van de Voorde P, Turner NM, Djakow J, et al. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation. 2021;161:327–87. https://doi.org/10.1016/j.resu....
16.
Sweet DG, Carnielli VP, Greisen G, et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome: 2022 Update. Neonatology. 2023;120(1):3–23. https://doi.org/10.1159/000528....
17.
Jeng MJ, Lee YS, Tsao PC, et al. Neonatal air leak syndrome and the role of high-frequency ventilation in its prevention. J Chin Med Assoc. 2012;75(11):551–59. https://doi.org/10.1016/j.jcma....
18.
Ma L, Yin M, Yang XL, et al. Risk factors for air leakage during invasive mechanical ventilation in pediatric intensive care units. Eur J Med Res. 2022;27(1):218. https://doi.org/10.1186/s40001....
19.
Liu K, Chen L, Xiong J, et al. HFOV vs CMV for neonates with moderate- to-severe perinatal onset acute respiratory distress syndrome (NARDS): a propensity score analysis. Eur J Pediatr. 2021;180(7):2155–64. https://doi.org/10.1007/s00431....
20.
Elgin TG, Berger JN, Thomas BA, et al. Ventilator Management in Extremely Preterm Infants. Neoreviews. 2022;23(10):661–76. https://doi.org/10.1542/neo.23....
21.
Hummler HD, Parys E, Mayer B, et al. Risk Indicators for Air Leaks in Preterm Infants Exposed to Restrictive Use of Endotracheal Intubation. Neonatology. 2015;108(1):1–7. https://doi.org/10.1159/000375....
22.
Trujillo MH, Fragachan CF, Tortoledo F. Cardiac Tamponade due to Pneumopericardium. Cardiology. 2005;105(1):34–36. https://doi.org/10.1159/000088....
23.
Kayashima K. Factors affecting survival in pediatric cardiac tamponade caused by central venous catheters. J Anesth. 2015;29(6):944–52. https://doi.org/10.1007/s00540....
24.
Meyer S, Ruffing S, Geipel M, et al. Something is up in the air: pneumo- thorax and pneumopericardium in a 29-week preterm infant. Wien Med Wochenschr. 2024;174(11–12):211–12. https://doi.org/10.1007/s10354....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.