Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
Clinical presentation and management of PANDAS Syndrome – Case Report
1
Student Scientific Association, Department of Paediatric Neurology, Medical University, Lublin, Poland
2
4th Clinical University Hospital, Medical University, Lublin, Poland
3
Department of Children’s Neurology, Department of Paediatric Neurology, University Children’s Hospital, Lublin, Poland
Corresponding author
Kamila Antonina Kapłon
Student Scientific Association, Department of Paediatric Neurology, Medical University,Lublin, Poland
Student Scientific Association, Department of Paediatric Neurology, Medical University,Lublin, Poland
J Pre Clin Clin Res. 2025;19(2):52-56
KEYWORDS
scarlet feverPANDAS syndromeGroup A Streptococcal InfectionAutoimmune neuropsychiatric disordersintravenous immunoglobulin (IVIG) therapy
TOPICS
ABSTRACT
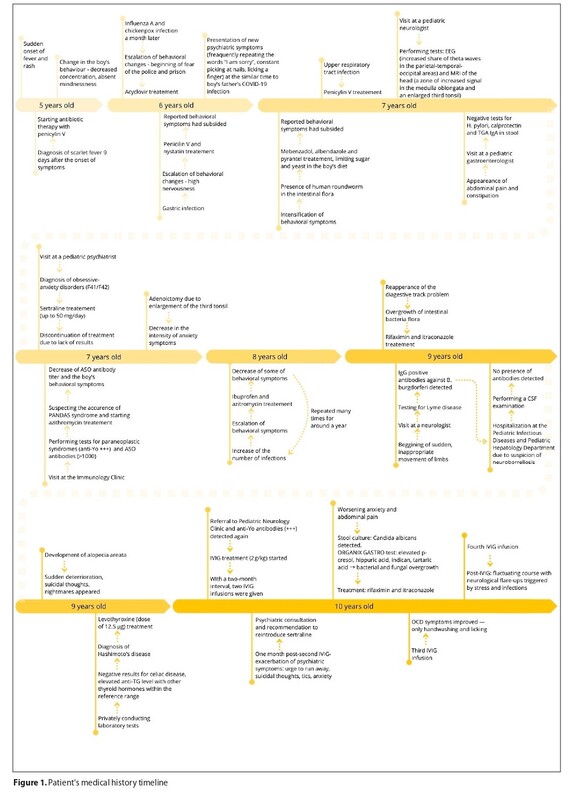
Autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) are difficult to recognize and diagnose. Symptoms are non-specific, appear suddenly, and may be related to a prior Group A beta-haemolytic streptococcal infection. Limited research complicates treatment. The case is presented of a 10-year-old boy with suspected PANDAS. Symptoms occurred after scarlet fever at the age of 5, which included sudden behavioural changes, decreased attention, and frequent dropping of objects. Over time, there were periods of worsening symptoms, especially during infections and stressful situations. Due to a positive titer of anti-Yo onconeural antibodies, IVIG therapy was initiated. Despite four series of treatment, the neurological symptoms did not significantly decrease. PANDAS remains a diagnostic and therapeutic challenge, requiring further research. It is important to emphasize the need for an interdisciplinary approach and new therapeutic strategies to improve patient outcomes.
Kapłon KA, Iwanicka K, Artemuk A, Pawelec K, Jóźwiak S, Ostolski M, Kamieniak A, Szukała K, Chrościńska-Krawczyk M. Clinical presentation
and management of PANDAS Syndrome – Case Report. J Pre-Clin Clin Res. 2025;19(2):52–56. doi:10.26444/jpccr/204548
REFERENCES (16)
1.
La Bella S, Attanasi M, Di Ludovico A, et al. Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS) Syndrome: A 10-Year Retrospective Cohort Study in an Italian Centre of Paediatric Rheumatology. Microorganisms. 2023;12(1):8. https://doi.org/10.3390/microo....
2.
LaRusso MD, Abadía-Barrero C, Developmental Impacts of PANS/ PANDAS and Inadequate Support for Children and Families. Child Psychiatry Hum Dev. 2024. https://doi.org/10.1007/s10578....
3.
Wilbur C, Bitnun A, Kronenberg S, et al. PANDAS/PANS in childhood: Controversies and evidence. Paediatr Child Health. 2019;24(2):85–91. https://doi.org/10.1093/pch/px....
4.
La Bella S, Scorrano G, Rinaldi M, et al. Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS): Myth or Reality? The State of the Art on a Controversial Disease. Microorganisms. 2023;11(10):2549. https://doi.org/10.3390/microo....
5.
Prato A, Gulisano M, Scerbo M, et al. Diagnostic Approach to Paediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections (PANDAS): A Narrative Review of Literature Data. Front Pediatr. 2021;9:746639. https://doi.org/10.3389/fped.2....
6.
Vreeland A, Calaprice D, Or‐Geva N, et al. Postinfectious inflammation, autoimmunity, and obsessive-compulsive disorder: sydenham chorea, paediatric autoimmune neuropsychiatric disorder associated with streptococcal infection, and paediatric acute-onset neuropsychiatric disorder. Developmental Neuroscience. 2023;45(6), 361–374. https://doi.org/10.1159/000534....
7.
Cocuzza S, Maniaci A, La Mantia I, et al. Obsessive-Compulsive Disorder in PANS/PANDAS in Children: In Search of a Qualified Treatment-A Systematic Review and Metanalysis. Children (Basel). 2022;9(2):155. https://doi.org/10.3390/childr....
8.
Sigra S, Hesselmark E, Bejerot S. Treatment of PANDAS and PANS: a systematic review. Neurosci Biobehav Rev. 2018;86:51–65. https://doi.org/10.1016/j.neub....
9.
Rea I, Guido CA, Spalice A. Clinical Features in Patients With PANDAS/ PANS and Therapeutic Approaches: A Retrospective Study. Front Neurol. 2021;12:741176. https://doi.org/10.3389/fneur.....
10.
Thienemann M, Murphy T, Leckman J, et al. Clinical Management of Paediatric Acute-Onset Neuropsychiatric Syndrome: Part I-Psychiatric and Behavioral Interventions. J Child Adolesc Psychopharmacol. 2017;27(7):566–573. https://doi.org/10.1089cap.201....
11.
Murphy ML, Pichichero ME. Prospective identification and treatment of children with paediatric autoimmune neuropsychiatric disorder associated with group A streptococcal infection (PANDAS). Arch Pediatr Adolesc Med. 2002;156(4):356–361. https://doi.org/10.1001/archpe....
12.
Prasad N, Johng S, Powell D, et al. Role of tonsillectomy and adenoidectomy in parental satisfaction of treatments for PANDAS Am J Otolaryngol. 2021;42(4):102963. https://doi.org/10.1016/j.amjo....
13.
Williams KA, Swedo SE, Farmer CA, et al. Randomized, Controlled Trial of Intravenous Immunoglobulin for Paediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections. J Am Acad Child Adolesc Psychiatry. 2016;55(10):860–867.e2. https://doi.org/10.1016/j.jaac....
14.
Younger DS, Xiaoling Ch. IVIg therapy in PANDAS: analysis of the current literature. J Neurol Neurosurg. 2016;3(3):125.
15.
Connelly-Smith L, Alquist CR, Aqui NA, et al. Guidelines on the Use of Therapeutic Apheresis in Clinical Practice – Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Ninth Special Issue. J Clin Apher. 2023;38(2):77–278. https://doi.org/10.1002/jca.22....
16.
Latimer ME, L’Etoile N, Seidlitz J, et al. Therapeutic plasma apheresis as a treatment for 35 severely ill children and adolescents with paediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. J Child Adolesc Psychopharmacol. 2015;25(1):70–5. https://doi.org/10.1089/cap.20....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.