Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Knowledge and attitude of primary healthcare workers towards rational prescription of Artemisinin-based combination therapy in the treatment of uncomplicated malaria in Ondo State, southwestern Nigeria
1
Department of Planning, Research and Statistics, State Ministry of Health, Lafia, Nasarawa State, Nigeria
2
School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia
3
Department of Pharmaceutics and Pharmaceutical Microbiology, Faculty of Pharmaceutical Science, Usmanu Danfodiyo University, Sokoto, Nigeria
4
Department of Community Medicine, Faculty of Clinical Sciences, Ladoke Akintola University of Science and Technology, Ogbomoso, Nigeria
5
Department of Pharmaceutics and Pharmaceutical Microbiology, Faculty of Pharmaceutical Sciences, Usmanu Danfodiyo University Sokoto, Nigeria
Corresponding author
J Pre Clin Clin Res. 2021;15(1):5-14
KEYWORDS
TOPICS
ABSTRACT
Introduction:
For an effective and desired outcome of therapy to be achieved, the technical capacity of the healthcare worker is a key factor. The aim of the study is to assess knowledge and attitudes of primary healthcare (PHC) workers towards rational artemisinin-based combination therapy (ACT) prescribed in the treatment of uncomplicated malaria.
Material and methods:
This is a descriptive cross-sectional survey in which a self-administered structured questionnaire was used. A combination of stratified and multistage sampling techniques where utilized in the selection of the healthcare workers (HCWs)
Results:
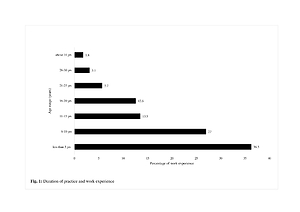
Of the 422 respondents, 100 (23.7%) were males and 322 (76.3%) were females. Respondents with less than five years in practice accounted for 36%, while 64% had six years and above of practice. Community health extension workers (CHEW) accounted for 54%,while 46% were either community health officers (CHO), nurses, midwives, Bachelors of Science (BSc) in community health, or with other qualifications. A total of 390 (92.4%) were aware of the availability of ACTs and used the malaria treatment protocols, whereas 28 (6.6%) still used monotherapy for simple malaria treatment, and 2.7% did not use any form of test before initiating treatment. Co-administration of non-ACTs with ACTs accounted for 12%, with 88% prescribing paracetamol with ACTs. 67% of the respondents required capacity building in rational ACT use.
Conclusions:
The majority of the respondents had the requisite knowledge and skills coupled with positive attitudes in prescribing ACTs. Some respondents could not distinguish between an ACTs and a monotherapy. This may affect the exact application of the malaria treatment protocols, especially at the PHC level.
For an effective and desired outcome of therapy to be achieved, the technical capacity of the healthcare worker is a key factor. The aim of the study is to assess knowledge and attitudes of primary healthcare (PHC) workers towards rational artemisinin-based combination therapy (ACT) prescribed in the treatment of uncomplicated malaria.
Material and methods:
This is a descriptive cross-sectional survey in which a self-administered structured questionnaire was used. A combination of stratified and multistage sampling techniques where utilized in the selection of the healthcare workers (HCWs)
Results:
Of the 422 respondents, 100 (23.7%) were males and 322 (76.3%) were females. Respondents with less than five years in practice accounted for 36%, while 64% had six years and above of practice. Community health extension workers (CHEW) accounted for 54%,while 46% were either community health officers (CHO), nurses, midwives, Bachelors of Science (BSc) in community health, or with other qualifications. A total of 390 (92.4%) were aware of the availability of ACTs and used the malaria treatment protocols, whereas 28 (6.6%) still used monotherapy for simple malaria treatment, and 2.7% did not use any form of test before initiating treatment. Co-administration of non-ACTs with ACTs accounted for 12%, with 88% prescribing paracetamol with ACTs. 67% of the respondents required capacity building in rational ACT use.
Conclusions:
The majority of the respondents had the requisite knowledge and skills coupled with positive attitudes in prescribing ACTs. Some respondents could not distinguish between an ACTs and a monotherapy. This may affect the exact application of the malaria treatment protocols, especially at the PHC level.
Baba Danjuma Oyinaka, Nura Muhammad Umar, Nafiu Aminu, Calistus A Akinleye, Tanko Nuhu. Knowledge and Attitude of Primary Healthcare
Workers towards Rational Prescription of Artemisinin-Based Combination Therapy in the Treatment of Uncomplicated Malaria in Ondo State
Southwestern Nigeria. J Pre-Clin Clin Res. 2021; 5–14. doi: 10.26444/jpccr/131762
REFERENCES (13)
1.
World Health Organization. World Malaria Report 2019. Geneva. WHO Regional Office for Africa. 2019. 1–232 p.
2.
Dawaki S, Al-Mekhlafi HM, Ithoi I, Ibrahim J, Atroosh WM, Abdulsalam AM, et al. Is Nigeria Winning The Battle Against Malaria? Prevalence, Risk Factors and KAP Assessment among Hausa Communities in Kano State. Malar J. 2016; 15(1): 1–14.
3.
World Health Organization. Antimalarial Drug Combination Therapy: Report of a WHO Technical Consultation. World Heal Organ Geneva. 2001; 36.
4.
Kuete T, Essono Mvoa E, Yinyang J, Epanya Priso A, Gougue Chamabe PC, Mpondo Mpondo E, et al. Pattern of Uncomplicated Malaria Treatment and Antimalarial Prescription Practices among Health.Workers in the Littoral Region of Cameroon: An Assessment of Ten Years Post-Malaria Treatment Policy Change. Pharmacol Pharm Pharm. 2016; 07(06): 217–225.
5.
Gbotosho GO, Sowunmi A, Happi CT, Okuboyejo TM. Therapeutic Efficacies of Artemisinin-based Combination Therapies in Nigerian Children with Uncomplicated Falciparum Malaria during Five Years of Adoption as First-line Treatments. Am J Trop Med Hyg. 2011; 84(6): 936–943.
6.
Meremikwu M, Alaribe A, Ejemot R, Oyo-Ita A, Ekenjoku J, Nwachukwu C, et al. Artemether-lumefantrine versus Artesunate plus Amodiaquine for Treating Uncomplicated Childhood Malaria in Nigeria: Randomized Controlled Trial. Malar J. 2006; 5: 1–6.
7.
Mannan AA, Malik EM, Ali KM. Antimalarial Prescribing and Dispensing Practices in Health Centres Of Khartoum State, 2003–04. East Mediterr Heal J. 2009; 15(1): 122–128.
8.
Mannan AA, Elmardi KA, Idris YA, Spector JM, Ali NA, Malik EM. Do Frontline Healthcare Providers Know Enough about Artemisinin-based Combination Therapy to Rationally Treat Malaria? A Cross-Sectional Survey in Gezira State, Sudan. Malar J. 2015; 14(1): 1–7.
9.
Toklu H. Promoting Evidence-Based Practice in Pharmacies. Integr Pharm Res Pract. 2015; 4: 127–131.
10.
Asibong U, Etokidem A, Akpan U, Archibong F. Malaria: Knowledge, Attitudes and Acceptances of Rapid Diagnostic Test amongst Primary Healthcare Workers in some Selected Local Government Areas, Lagos State. Public Heal Res. 2019; 9(1): 13–21.
11.
Ndibuagu EO. Use of Malaria Rapid Diagnostic Tests among Medical Doctors in a Tertiary Hospital, South East Nigeria. Health. 2018; 10(07): 971–984.
12.
Nag S, Ursing J, Rodrigues A, Crespo M, Krogsgaard C, Lund O, et al. Proof of Concept: Used Malaria Rapid Diagnostic Tests Applied for Parallel Sequencing for Surveillance of Molecular Markers of Antimalarial Resistance in Bissau, Guinea-Bissau during 2014–2017. Malar J. 2019; 18(252): 1–13.
13.
Elmannan AAA, Elmardi KA, Idris YA, Spector JM, Ali NA, Malik EM. Antimalarial Prescribing Practices in Sudan Eight Years after Introduction of Artemisinin-based Combination Therapies and Implications for Development of Drug Resistance. BMC Pharmacol Toxicol. 2015; 16(1).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.