Online first
About the Journal
Current issue
Archive
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Office
Editorial Board
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Polydioxanone for orbital reconstruction – an ARRIVE-guided preclinical assessment of its inflammatory profile compared to titanium
1
Department of Diagnostics and Surgery, São Paulo State University (Unesp), School of Dentistry, Araraquara, São Paulo, Brazil
2
School of Dentistry, Federal University, Alagoas (UFAL), Brazil
Corresponding author
Luiz Henrique Godoi Marola
Department of Diagnostics and Surgery, São Paulo State University (Unesp), School of Dentistry, Humaitá, 1680, 14801-385 Araraquara, Brazil
Department of Diagnostics and Surgery, São Paulo State University (Unesp), School of Dentistry, Humaitá, 1680, 14801-385 Araraquara, Brazil
J Pre Clin Clin Res. 2025;19(2):64-69
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Polydioxanone (PDO), a biodegradable synthetic polymer, has been proposed for small orbital reconstructions due to its absorbable nature. However, past findings have raised concerns about its inflammatory response, warranting further investigation. The aim of this study is to evaluate the inflammatory profile and behaviour of periorbital tissue in rabbits using a PDO membrane.
Material and methods:
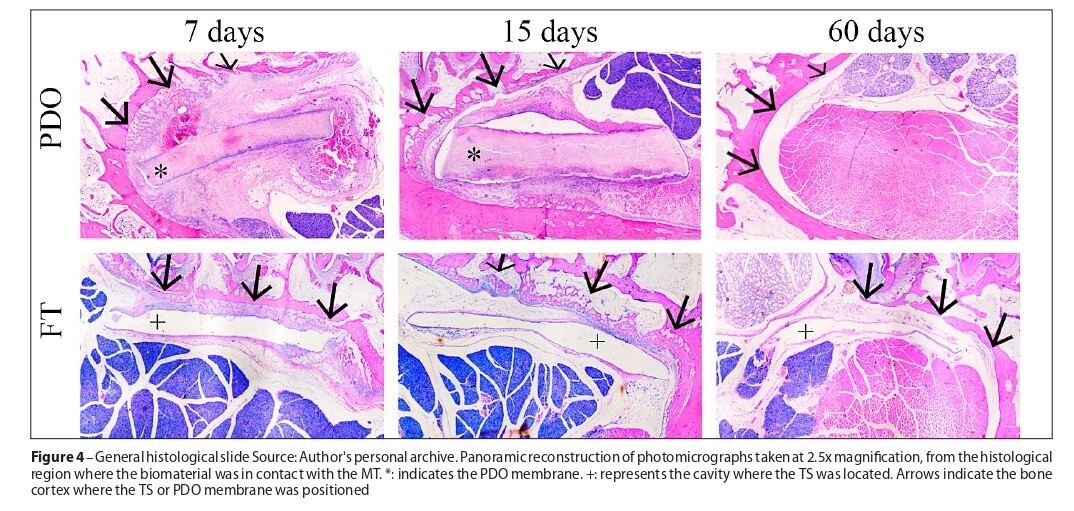
The trial was carried out in 17 male rabbits of the species Oryctolagus Cunilicus, in which one of the orbits was submitted to surgical exposure and positioning a PDO membrane (intervention). In the contralateral orbit, a titanium sheet (TS) was positioned (positive control). The orbits were evaluated to identify the inflammatory profile (neutrophils, plasma cells, lymphocytes, and blood vessels) by histometry at 7, 15, and 60 days.
Results:
The PDO group had more plasma cells in the 7 days than the titanium group (p = 0.012). In the 15 days, the PDO group had a higher number of lymphocytes (p = <.001), neutrophils (p = <.001), and plasma cells (p = <0.004) compared to the titanium group. Analysis of the granulation tissue area revealed a higher mean around the PDO in the periods of 7 and 15 days (p = 0.009 and p = <.001). PDO assessment did not suffer significant changes between the periods, and no remnants of the membrane were observed at 60 days. In contrast, the titanium group showed a significant decrease between 7–15 days (p = 0.041), and no changes between 15–60 days.
Conclusions:
Considering the limitations, it was concluded that the PDO membrane caused a greater inflammatory process than TS, however, this inflammation did not extend to adjacent periorbital tissues or result in relevant clinical changes during post-operative follow-up.
Polydioxanone (PDO), a biodegradable synthetic polymer, has been proposed for small orbital reconstructions due to its absorbable nature. However, past findings have raised concerns about its inflammatory response, warranting further investigation. The aim of this study is to evaluate the inflammatory profile and behaviour of periorbital tissue in rabbits using a PDO membrane.
Material and methods:
The trial was carried out in 17 male rabbits of the species Oryctolagus Cunilicus, in which one of the orbits was submitted to surgical exposure and positioning a PDO membrane (intervention). In the contralateral orbit, a titanium sheet (TS) was positioned (positive control). The orbits were evaluated to identify the inflammatory profile (neutrophils, plasma cells, lymphocytes, and blood vessels) by histometry at 7, 15, and 60 days.
Results:
The PDO group had more plasma cells in the 7 days than the titanium group (p = 0.012). In the 15 days, the PDO group had a higher number of lymphocytes (p = <.001), neutrophils (p = <.001), and plasma cells (p = <0.004) compared to the titanium group. Analysis of the granulation tissue area revealed a higher mean around the PDO in the periods of 7 and 15 days (p = 0.009 and p = <.001). PDO assessment did not suffer significant changes between the periods, and no remnants of the membrane were observed at 60 days. In contrast, the titanium group showed a significant decrease between 7–15 days (p = 0.041), and no changes between 15–60 days.
Conclusions:
Considering the limitations, it was concluded that the PDO membrane caused a greater inflammatory process than TS, however, this inflammation did not extend to adjacent periorbital tissues or result in relevant clinical changes during post-operative follow-up.
Department of Diagnostics and Surgery, São Paulo State University (Unesp), School of Dentistry, Araraquara, São Paulo, Brazil
REFERENCES (26)
1.
Marola LHG, Cassol J, Burigo F, Bomente FF, Chiarelli M. Etiology of facial trauma: an in-depth analysis of cases occurred in Florianópolis, SC from 2016 to 2019. Brazilian J Oral Maxilofac Surg. 2021;21:12–8.
2.
Marola LHG, Torres LHS, Mochizuki Junior C, Marinho BD, Chiarelli M, Pereira Filho VA. What solid evidence do systematic reviews provide about post-traumatic orbital reconstruction materials? An overview of systematic reviews. Rev Cient Multidiscip Núcleo Conhec. 2024;07:47–81.
3.
Birkenfeld F, Behrens E, Kern M, Gassling V, Wiltfang J. Mechanical properties of collagen membranes: Are they sufficient for orbital floor reconstructions? J Cranio-Maxillofacial Surg. 2015;43:260–3.
4.
Foletti JM, Scolozzi P. Severe distortion of an orbital titanium mesh implant after recurrent facial trauma: a potential threat to the orbital contents? Br J Oral Maxillofac Surg. 2017;55:836–8.
5.
Foletti JM, Martinez V, Haen P, Godio-Raboutet Y, Guyot L, Thollon L. titanium mesh for orbital floor reconstruction in case of trauma recurrence. J Stomatol Oral Maxillofac Surg. 2019;120:91–4.
6.
Jaquiéry C, Aeppli C, Cornelius P, Palmowsky A, Kunz C, Hammer B. Reconstruction of orbital wall defects: critical review of 72 patients. Int J Oral Maxillofac Surg. 2007;36:193–9.
7.
Boro S, Suri MP, Mathew AK. PDS Plate Versus Bone Graft in Orbital Floor Reconstruction: A Prospective Study to Identify the Better Alternative. Indian J Otolaryngol Head Neck Surg. 2022;74:S4699–705.
8.
Winnand P, Ooms M, Ayoub N, Schick D, Von Beck FP, Holzle F, et al. reconstruction of the orbital geometry after isolated orbital floor fractures. Eur J Trauma Emerg Surg. 2024;50:2579–86.
9.
Ramesh S, Hubschman S, Goldberg R. Resorbable Implants for Orbital Fractures: A Systematic Review. Ann Plast Surg. 2018;81:372–9.
10.
Kontio R, Suuronen R, Salonen O, Paukku P, Konttinen YT, Lindqvist C. Effectiveness of operative treatment of internal orbital wall fracture with polydioxanone implant. Int J Oral Maxillofac Surg. 2001;30:278–85.
11.
du Sert NP, Hurst V, Ahluwalia A, Alam S, Avey MT, Baker M, et al. The arrive guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol. 2020;18:1–12.
12.
Lee JM, Baek S. Antiadhesive effect of mixed solution of sodium hyaluronate and sodium carboxymethylcellulose after blow-out fracture repair. J Craniofac Surg. 2012;23:1878–83.
13.
Bizelli VF, Viotto AHA, Delamura IF, Baggio AMP, Ramos EU, Faverani LP, et al. Inflammatory Profile of Different Absorbable Membranes Used for Bone Regeneration: An In Vivo Study. Biomimetics. 2024;9:431–44.
14.
Liao T, Li N. Single-Perspective Warps in Natural Image Stitching. EEE Trans Image Process. 2020;29:724–35.
15.
Aral AM, Özmen S, Uygur S, Kaya B, Coskun N, Ömeroglu S, et al. Comparison of resorbable mesh (Poly l-lactide/glycolic acid) and porous polyethylene in orbital floor fractures in an experimental model. Plast Surg. 2017;25:163–70.
16.
Zheng YX, Wang J, Lin HT, Li L. Reconstruction of orbital defect in rabbits with composite of calcium phosphate cement and recombinant human bone morphogenetic protein-2. Chin Med J (Engl). 2010;123:3658–62.
17.
Görgülü T, Akçal A, Uğurlu K. Use of human nail for reconstruction of the orbital floor: an experimental study in rabbits. Br J Oral Maxillofac Surg 2016;54:664–8.
18.
Gu RD, Xiao F, Wang L, Sun KJ, Chen LL. Biocompatibility of polyetheretherketone for the treatment of orbital bone defects. Int J Ophthalmol. 2020;13:725–30.
19.
Ho Han H, Yun S, Won JY, Lee JS, Kim KJ, Park KH, et al. Orbital wall reconstruction in rabbits using 3D printed polycaprolactone-β-tricalcium phosphate thin membrane. Mater Lett 2018;218:280–4.
20.
Mariano J, Costa C, Patrocínio LG, Rossi R De, Amorim ÂBC, Patrocínio JA. Utilização da Esclera Bovina para Correção de Fratura em Assoalho de Órbita de Coelhos Bovine Sclerae Graft for Orbital Floor Fracture n Rabbits. Animals. 2005;9:181–9.
21.
Bonaud A, Khamyath M, Espéli M. The cellular biology of plasma cells: Unmet challenges and opportunities. Immunol. Lett 2023; 254:6–12.
22.
Saska S, Pilatti L, De Sousa Silva ES, Nagasawa MA, Câmara D, Lizier N,et al. Polydioxanone-based membranes for bone regeneration. Polymers (Basel). 2021;13:1685.
23.
Dietz A, Dacho A, Althof F, Ziegler CM, Kolling G, H VB, et al. Effectiveness of a new perforated 0.15 mm poly-p-dioxanon-foil versus titanium-dynamic mesh in reconstruction of the orbital floor. J Cranio- Maxillofacial Surg. 2001;29:82–8.
24.
Becker ST, Terheyden H, Fabel M, Kandzia C, Möller B, Wiltfang J. Comparison of collagen membranes and polydioxanone for reconstruction of the orbital floor after fractures. J Craniofac Surg. 2010;21:1066–8.
25.
Beck-Broichsitter BE, Acar C, Kandzia C, Jochens A, Wiltfang J, Becker ST. Reconstruction of the orbital floor with polydioxanone: A long-term clinical survey of up to 12 years. Br J Oral Maxillofac Surg. 2015;53:736–40.
26.
Jank S, Emshoff R, Schuchter B, Strobl H, Brandlmaier I, Norer B. Orbital floor reconstruction with flexible Ethisorb patches: A retrospective long-term follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:16–22.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.